Summer 2025 (Volume 35, Number 2)
Rule Out
CNS Vasculitis
By Kim Legault, MD, MSc, FRCPC
Download PDF
When faced with the referral stating: “Please rule out central nervous system vasculitis”, all rheumatologists know that it’s time to get their thinking caps on! Assessing a patient for the presence of central nervous system vasculitis (CNS-V) is challenging due to the lack of specificity of our standard diagnostic tools. Diagnosis requires careful review of history, physical exam, imaging, cerebrospinal fluid (CSF) analysis, laboratory findings, serologies, and, if needed, pathology of brain tissue. Collaboration with other specialists, particularly neurologists, neuroradiologists, and neurosurgeons is critical to properly interpret investigations and explore the non-rheumatological conditions on the differential diagnosis. This can be a daunting task, and having an organized approach to the mimickers and classification of CNS-V is critical.
Consider following these steps to approach
these consults:
1) Categorize the location of the potential neuroinflammation:
Is it Vascular, Parenchymal, or Pachymeningeal?
(or a combination). This requires neuroimaging.
- Brain magnetic resonance imaging (MRI) allows assessment for the presence of parenchymal, pachymeningeal/leptomeningeal inflammation, and/or evidence of changes that suggest vascular compromise.
- Parenchymal inflammation can have a variety of different appearances, though in general it will present as hyperintense signal on T2 and FLAIR sequences. Administration of gadolinium can increase the sensitivity, and enhancement can indicate “activity” of specific lesions.
- “Demyelination” is a specific subtype of parenchymal inflammation. Inflammatory processes that disrupt the myelin sheath in disorders such as multiple sclerosis lead to a specific pattern of white matter hyperintensities on MRI. There are specific rheumatological diagnoses that can lead to this type of inflammatory picture, particularly MS-like presentations of Sjogren’s disease, and neuromyelitis optica spectrum disease.
- Pachymeningeal inflammation of the dura mater is seen as thickening and enhancement on MRI. This can be seen in isolation or with other vascular or parenchymal findings.
- Vascular compromise to the brain will manifest as a stroke on imaging, if the vessel is large enough. However if the vasculitis affects very small vessels (e.g., anti-neutrophil cytoplasmic antibody (ANCA) vasculitis with CNS involvement), it may manifest only as an increased number of white matter hyperintensities on T2 and FLAIR sequences, a finding which is non-specific, and can be indistinguishable from parenchymal inflammation, non-inflammatory small vessel microvascular changes (e.g., from diabetes, hypertension, smoking), migraine, or normal aging.
- Neurovascular imaging – computed tomography (CT) angiography (or magnetic resonance (MR) angiography) of the cerebral vessels
- Will show stenosis, tortuosity, occlusion of affected vessels, provided the vessels affected are sufficiently large – small vessel CNS-V can be below the resolution of angiography.
2) Develop a differential diagnosis based on the location of the potential neuroinflammation, considering non-inflammatory and inflammatory pathologies:
The differential diagnosis for the appearance of inflammation in each of these locations is outlined in figure 1.
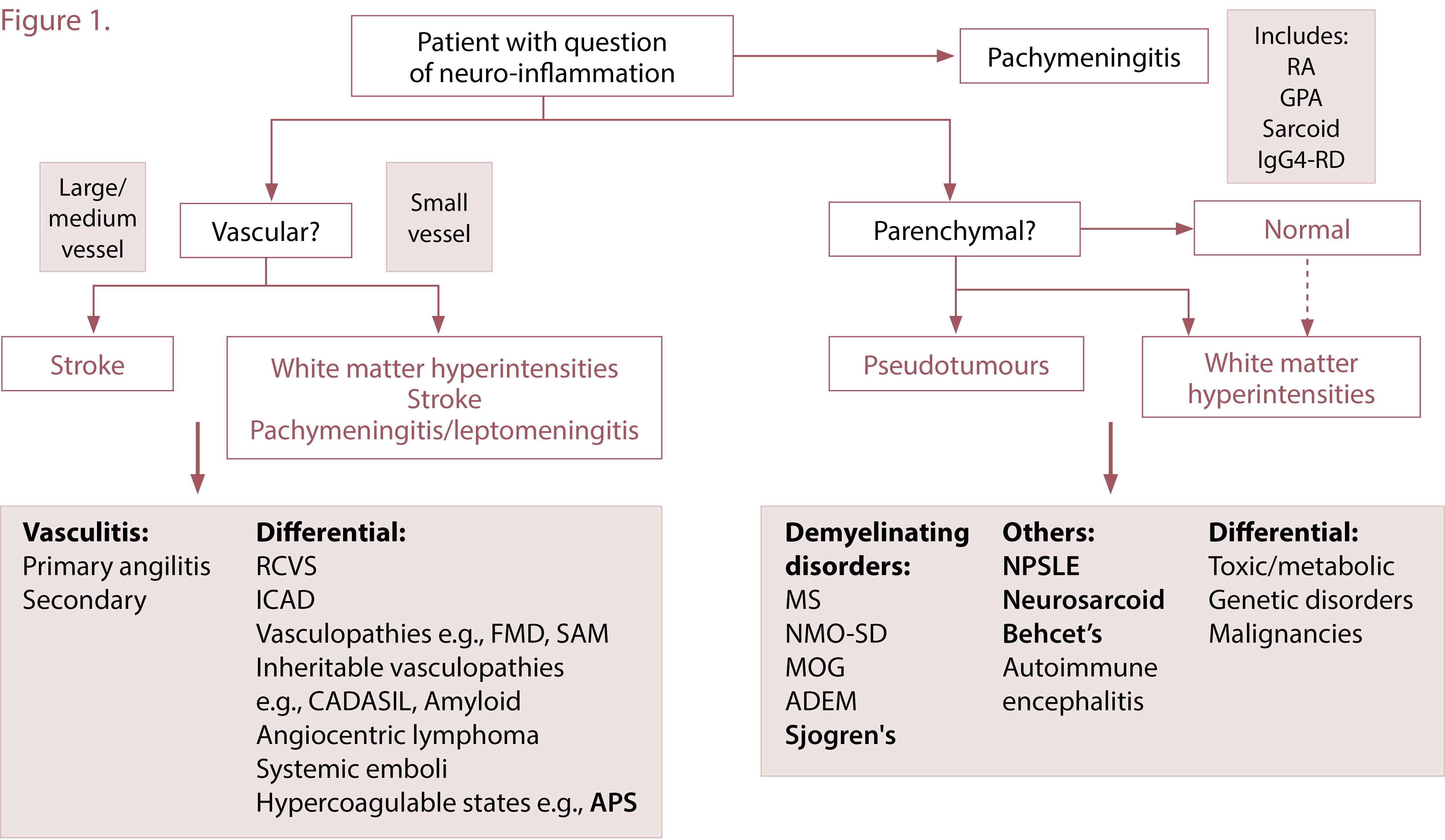
Parenchymal
- For parenchymal CNS white matter abnormalities, the differential includes:
- Non-inflammatory: toxic/metabolic conditions, genetic disorders e.g., leukodystrophy, and malignancies such as lymphoma. It is critical to partner with the neurology team in order to assess for these entities.
- Inflammatory: Neuropsychiatric manifestations of connective tissue disease such as systemic lupus erythematosus, sarcoidosis, and Behcet’s. These can be investigated through the rheumatologist’s assessment of whether there are signs or symptoms of active disease, whether serologies are supportive of a diagnosis, or whether there is a site for biopsy in other organ systems.
Pachymeningeal
-
Non-inflammatory: malignancy.
-
Inflammatory: IgG4-related disease, rheumatoid arthritis (RA), ANCA vasculitis, sarcoidosis, idiopathic. The rheumatologist can assess for extra-neurological manifestations of these conditions to come to a presumed diagnosis, or to access sites for relevant biopsies outside of the CNS if possible.
Vascular
- Non-inflammatory mimickers: reversible cerebral vasoconstriction syndrome, intracranial atherosclerotic disease (ICAD), vasculopathies e.g., fibromuscular dysplasia, vascular Ehlers-Danlos, inheritable vasculopathies such as CADASIL, hereditary cerebral amyloid, angiocentric lymphoma, and hypercoagulable states. Differentiation of these conditions from vasculitis can be challenging, particularly in the setting of ICAD. Many require experienced neuroradiology assessment.
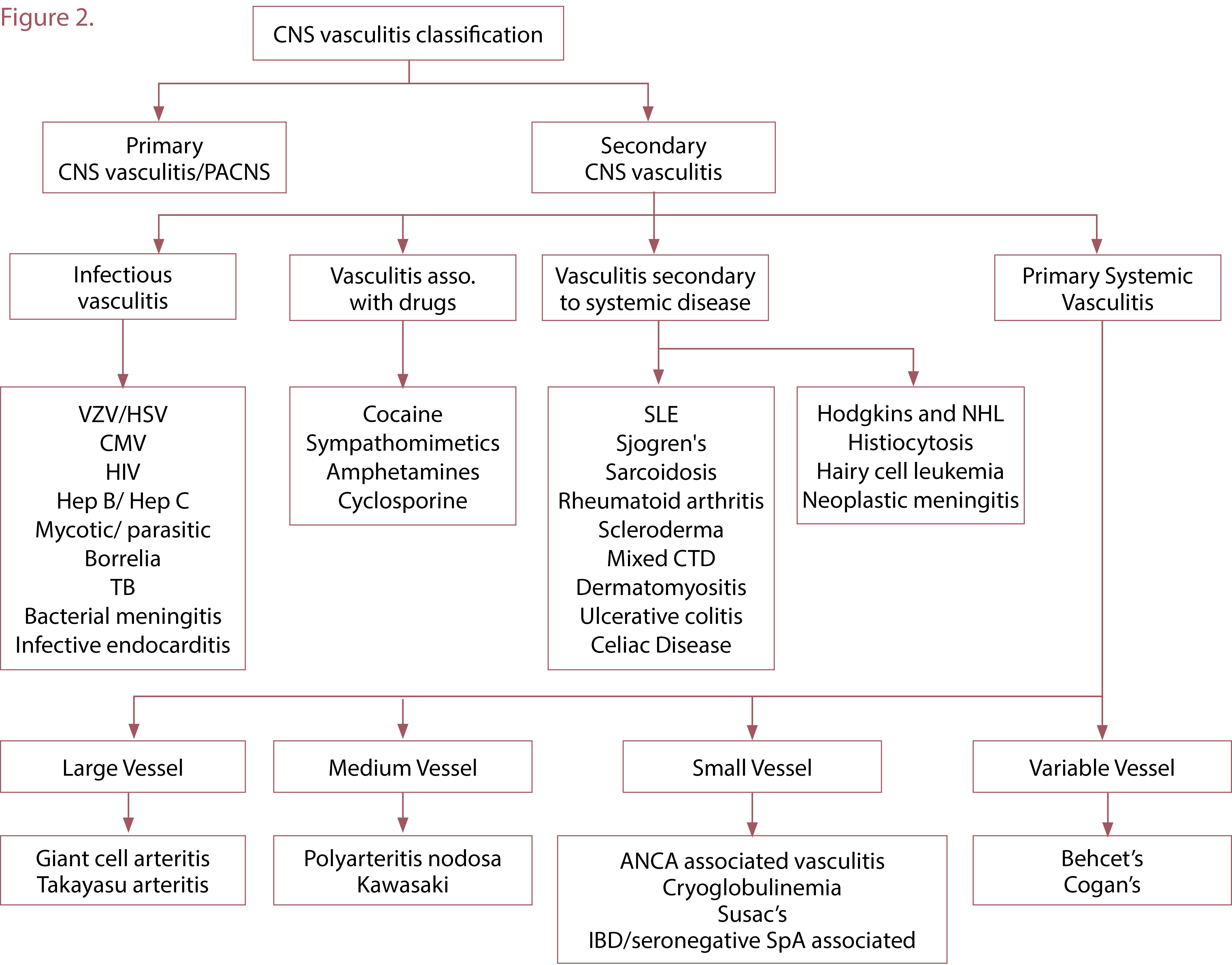
- Inflammatory vasculitis (i.e., CNS-V):
- Primary CNS-V: rare disorder of isolated vasculitis in the CNS without systemic vasculitis
- Secondary CNS-V: vascular inflammation secondary to another systemic process
(See figure 2 for full differential)
- Infectious
- Drug-induced
- Vasculitis associated with other systemic diseases – malignancies, autoimmune conditions
- Primary systemic vasculitis with CNS involvement
3) In the setting of a vascular process, attempt to differentiate inflammatory from non-inflammatory vasculopathies, as follows.
Features that can assist include:
- Clinical assessment – CNS-V can result in subacute headache and cognitive or behavioural changes
- Symptoms and signs of associated infectious, neoplastic, autoimmune processes can be found
- Labs/Serologies - for potential associated infections, rheumatological conditions
- CSF analysis - can show elevated protein, a mild pleiocytosis (<50 cells; higher levels are more consistent with infection or lymphoma), and oligoclonal bands
- Oligoclonal bands are indicative of immunoglobulins in the CSF space
- They are collected from CSF with a paired serum sample.
- If they are “non-matching”, then they are only in CSF space, and indicate an inflammatory process isolated to the CSF with intrathecal production of immunoglobulin. This is classically seen in MS; can be seen in primary CNS-V.
- If they are “matching” this indicates a systemic process where immunoglobulin have reached the CSF space through a breakdown in the blood-brain barrier, which suggests a systemic inflammatory disorder. Can be seen with many processes, e.g., secondary CNS-V such as ANCA vasculitis; neuropsychiatric lupus; infections, etc.
Imaging
-
Pachy- or leptomeningeal enhancement are associated with CNS-V.
-
Vessel wall imaging: Both ICAD and CNS-V can show abnormalities in medium vessels on angiography; MRI with vessel wall imaging targeting an affected vessel can be helpful to differentiate – CNS-V shows concentric vessel wall enhancement (circumferential inflammation of the vessel wall of an affected vessel) whereas ICAD generally shows eccentric enhancement (asymmetrical plaque deposition).
Biopsy
-
If diagnostic uncertainty remains after these tests, consider brain biopsy, of leptomeninges and cortex – targeting an affected site that is accessible as per the neurosurgery team. This is diagnostic in ~90% of cases, with 30-50% of cases showing an alternative diagnosis. Sensitivity decreases if non-targeted biopsies (non-dominant temporal lobe) are performed.
It is through a careful process of assessment of all of the available diagnoses fitting a patient’s particular clinical scenario, as well as multispecialty review considering all of the appropriate differential diagnoses, where the best diagnosis possible is achieved. Therapy can then be targeted to this diagnosis. At follow-up assessment, if a patient is not responding as expected to a particular course of therapy, it is always important to reconsider the diagnosis, and to consider additional or repeat diagnostic tests to increase yield.
This approach will assist rheumatologists in having a framework to use to consider patients with the question of central nervous system vasculitis.
Kim Legault, MD, MSc, FRCPC
Program Director, Rheumatology Residency Program
McMaster Professorship in Rheumatology Education
Associate Professor, Division of Rheumatology, Department of Medicine
McMaster University
Hamilton, Ontario
|
