Spring 2025 (Volume 35, Number 1)
“Hydrostomia”: The Art and Science for Relief of Dry Mouth
By Leslie P. Laing, BSc, BEd, MSc, PhD (Microbiology and Immunology), DDS, MSc (Prosthodontics), FRCD(C), FAP
Download PDF
With apologies to William Shakespeare who wrote “A rose by any other name would smell as sweet”1, we might paraphrase by saying “Saliva by any other name would still be considered yucky”. Saliva does not have a very endearing reputation and is often derogatorily called “spit”, “slobber”, “drool”, “spittle”, or “dribble”. Saliva is that seemingly innocuous fluid that we really don’t like to think about and tend to take for granted. Yet it is vital to our daily activities. It preserves and maintains oral health and function; aids digestion; contributes to taste perception; facilitates communication; protects oral tissues from desiccation, microbial penetration, or ulceration; stimulates soft tissue repair; provides comfort while wearing dentures through its lubricating ability; and protects against caries by protecting dental surfaces, neutralizing acids, acting as a buffer, diluting acids, and promoting remineralization. Yet in the words of fellow Canadian Joni Mitchell: “Don’t it always seem to go that you don’t know what you’ve got ‘til it’s gone”2. When it has gone or its production is diminished, it reduces the quality of life beyond measure. The dry mouth sufferer may still look the same externally, but numerous aspects of the simple joys of life are hindered without it: socializing with family and friends, chatting, eating together, tasting, etc. And then to add insult to real injury, rampant caries may result, despite using all manner of oral hygiene products and techniques.
Dry mouth is associated with several auto-immune diseases, such as the most notable one Sjögren’s Disease (SjD), but also systemic lupus erythematosus (SLE), scleroderma, diabetes, graft-versus-host disease, rheumatoid arthritis (RA), and primary biliary cholangitis; with immunotherapy/radiation therapy for head/neck cancers; with over 500 common therapeutic medications, and with smoking marijuana which can lead to “cotton mouth”. Various terms have been used to define dry mouth and dysfunction of the salivary glands3:
Salivary gland hypofunction is an objectively decreased saliva secretion (i.e. below normal secretion), which is measured by salivary flow rate (SFR) such that the unstimulated or resting SFR is less than 0.1 mL/min (normal ~ 0.3 mL/min), and the stimulated SFR is less than 0.5 mL/min (normal 1-2 mL/min). Xerostomia is the subjective sensation of dry mouth. This is the patient’s perception that their mouth is dry, yet this may not be obvious upon intra-oral examination, since the extent of the dryness may be affected by factors other than salivary flow rates3. The diagnostic term hyposalivation is used when saliva secretion becomes pathologically low, as measured objectively.
Before resorting to pharmaceutical intervention, the following simple tricks and tips can aid in relieving dry mouth, i.e., “hydrostomia”.
1. Massage:
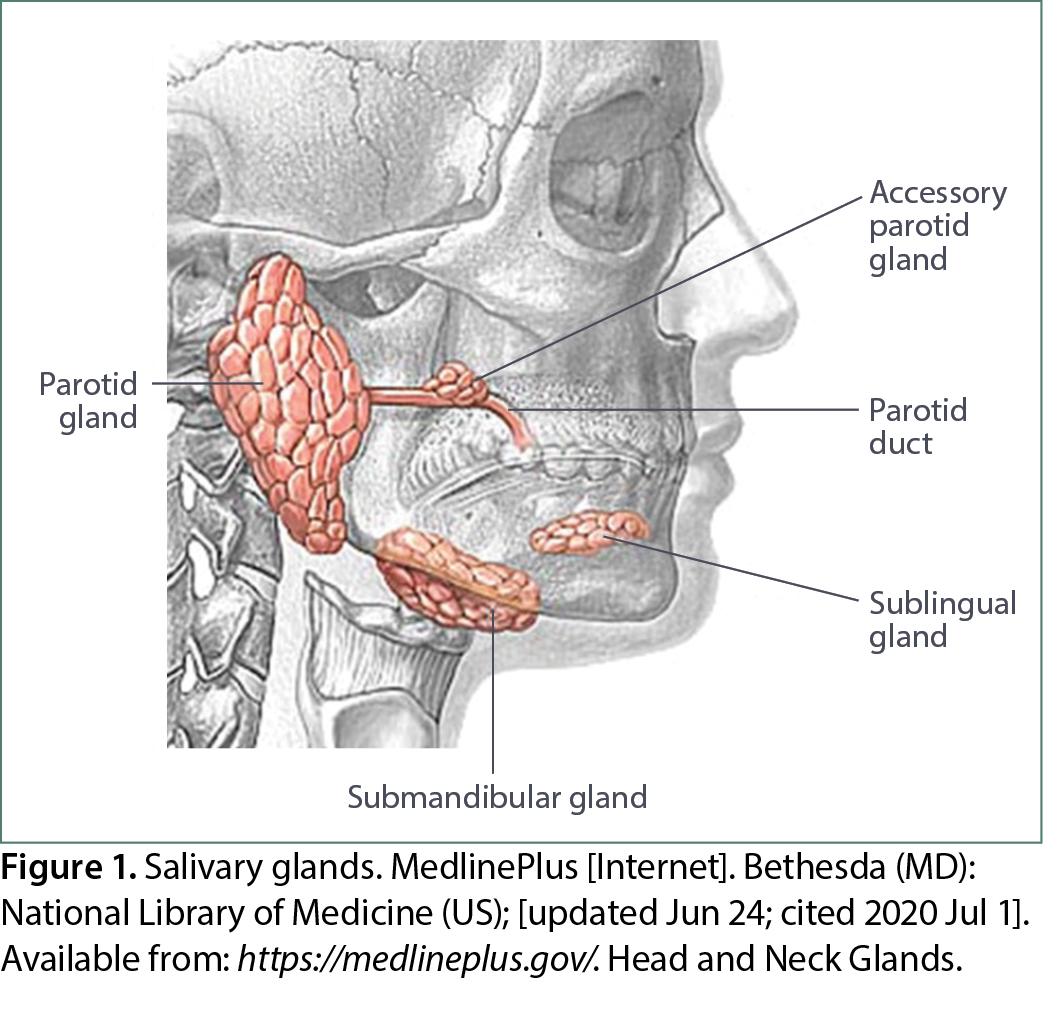
a. The major salivary glands. The largest of the major salivary glands, the parotid glands (Figure 1) are massaged by placing fingers on the cheeks and milking the glands in an anterior direction. This aids the flow of aqueous serous saliva through the Stenson duct. Similarly, viscous mucous saliva can be released from the mid-sized submandibular glands along and below the mandible’s lower border, emptying into Wharton’s duct. The small sublingual glands can be massaged intra-orally in a rather discrete manner by running the tongue from side to side along the floor of the mouth where the two soft pillow-like structures are located. Since this can be done with a closed mouth, with no one knowing you are doing this, it can be considered the “oral Kegels”.
b. The minor salivary glands. Even the minor salivary glands in the lips and gingival tissues can be massaged using a supersoft toothbrush with thousands of polyester filaments. The brush is gently held like a pen at a 45-degree angle with half the bristles on the gums and half on the teeth, then moved in small circles around the teeth. Even without water or toothpaste, saliva will be stimulated. Alternatively, electric water flossers can be used by aiming the tip of the device toward the teeth and directing the gentle flow of water at a 90-degree angle to the gumline.
2. Use sugar-free, xylitol-containing gum or lozenges. The mechanical stimulation of chewing gum or sucking on lozenges will stimulate saliva release. Choose those products sweetened with the sugar-substitute xylitol which has the added benefit of reducing caries4-6. Avoid sugar-free products containing aspartame which tends to dry the mouth even more.
3. Use herbal lollipops sweetened with licorice root extract. A unique delivery system of licorice root extract (LRE) in the form of a lollipop in a regime involving twice daily usage for 10 days has been shown to cause a marked reduction of salivary Strep. mutans, the micro-organism frequently associated with dental caries7. LRE has potentially beneficial effects in the treatment of cancer, atherosclerosis, gastric ulcers, hepatitis, autoimmune diseases (Crohn’s disease, lupus, scleroderma, rheumatoid arthritis), and oral disease (caries)7,8. The lollipop format has the added benefit of a handle to hold for those patients who have undergone surgical procedures for head and neck cancer where maintaining a lozenge or gum in the mouth is almost impossible.
4. Use a small, smooth item as an alternative to gum or lozenges. This can take the form of a cherry or olive pit, a plastic button or commercially available chewing device designed for this purpose, or even a pebble9-13. Any of these can be held “chipmunk-like” in and moved around the mouth, thereby stimulating the mechanoreceptors in gingival tissues and resulting in increased saliva production.
5. Drink green tea. Green tea polyphenols have been shown to reduce the risk and severity of cardiovascular disease, dental cavities, eye diseases, kidney stones, infectious diseases, and cancer while improving bone density, immune response, and cognitive function14,15. Drinking green tea has been shown to produce a clinically significant increase in salivary flow rate and a statistically significant decrease in salivary viscosity in patients with SjD7,15.
Additionally, as long as the tea is not too hot, the vessel holding it can be used as a warm compress for the parotid gland.
6. Be moderate in water drinking but stay hydrated. Water is not substantive in that it neither remains in the mouth nor lubricates the mouth or throat. Drinking a glass of water is preferable to numerous sips of water since what little saliva is present is swallowed along with the water. Instead, patients can suck on ice chips that have a longer “staying power”. An atomizer filled with water or a water: oil mixture with olive or coconut oil can be useful to spray at the back of the throat.
7. Wear removable prosthetic devices. These can be in the form of removable dentures, stabilization appliances, or night guards. By providing a replacement for missing teeth along with the denture bases that hug the edentulous ridges, careful prosthodontic treatment may increase stimulated and unstimulated (resting) SFR by allowing more frequent or forceful mastication and stimulation of mechanoreceptors in the oral mucosa under the denture base which a fixed solution (i.e., one that is not removable by the patient) cannot provide.16-21
8. Oil-pull with virgin coconut oil (VCO). Oil pulling, a traditional Ayurvedic technique dating back 3000-5000 years as a remedy for numerous oral ailments22, can help relieve dry mouth. In as little as three weeks the technique has been shown to reduce levels of both decay-associated Strep. mutans and yeast by 100-fold23,24. Patients also reported that their gums no longer bled when they flossed their teeth; they no longer noted a sourdough smell; they could taste their food again; and their teeth looked brighter. The oil has been shown to prevent the binding of bacteria to tooth surfaces and to have a bactericidal effect. Oil pulling is an adjunct to regular oral care and can be easily performed by placing one-half teaspoon of solid VCO in the mouth, pulling and pushing it through the teeth (i.e., swishing) for about 90 seconds, then spitting it out. The process can be repeated several times over a 15-20-minute period in keeping with the original timeframe.
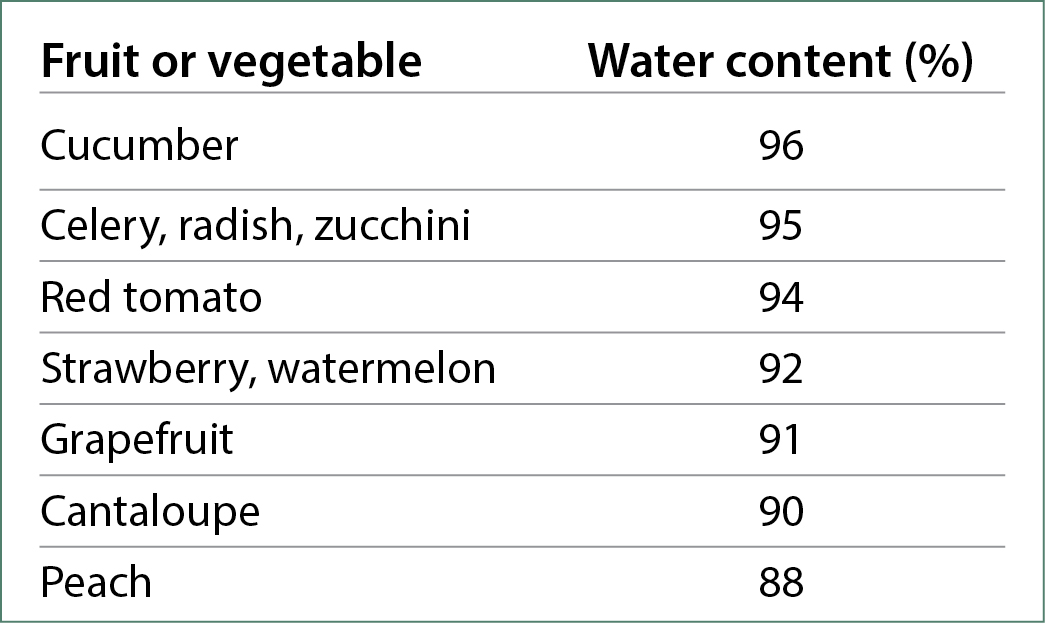
9. Consume Hydrating Foods. Most of our foods contain water which helps us stay hydrated. Due to their significant water content, fruits and vegetables serve as excellent substitutes for hydration25. Additionally, the act of chewing these foods can enhance saliva production through mechanical stimulation.
10. Try commercially available remoisturizing or remineralizing aids for home use. There are numerous commercially available products with claims of remoisturizing the mouth. They are available in various formats: gel, spray, toothpaste, mouth rinse, as well as disks or strips that adhere to the upper back soft tissue of the molar region. It is important to determine the pH of these products before use since some of the more familiar ones have a pH close to 326-28, comparable to that of lemons. While these low pH products may be great at stimulating saliva, they are also effective at eroding enamel. Perhaps it is best to save some money and just think of lemons and their “pucker power”. Remineralizing aids are also available with high fluoride or hydroxyapatite content and come in the form of toothpastes, rinses, or varnishes.
A Final Word on the Application of 38% Silver Diamine Fluoride (SDF): “Black Magic”
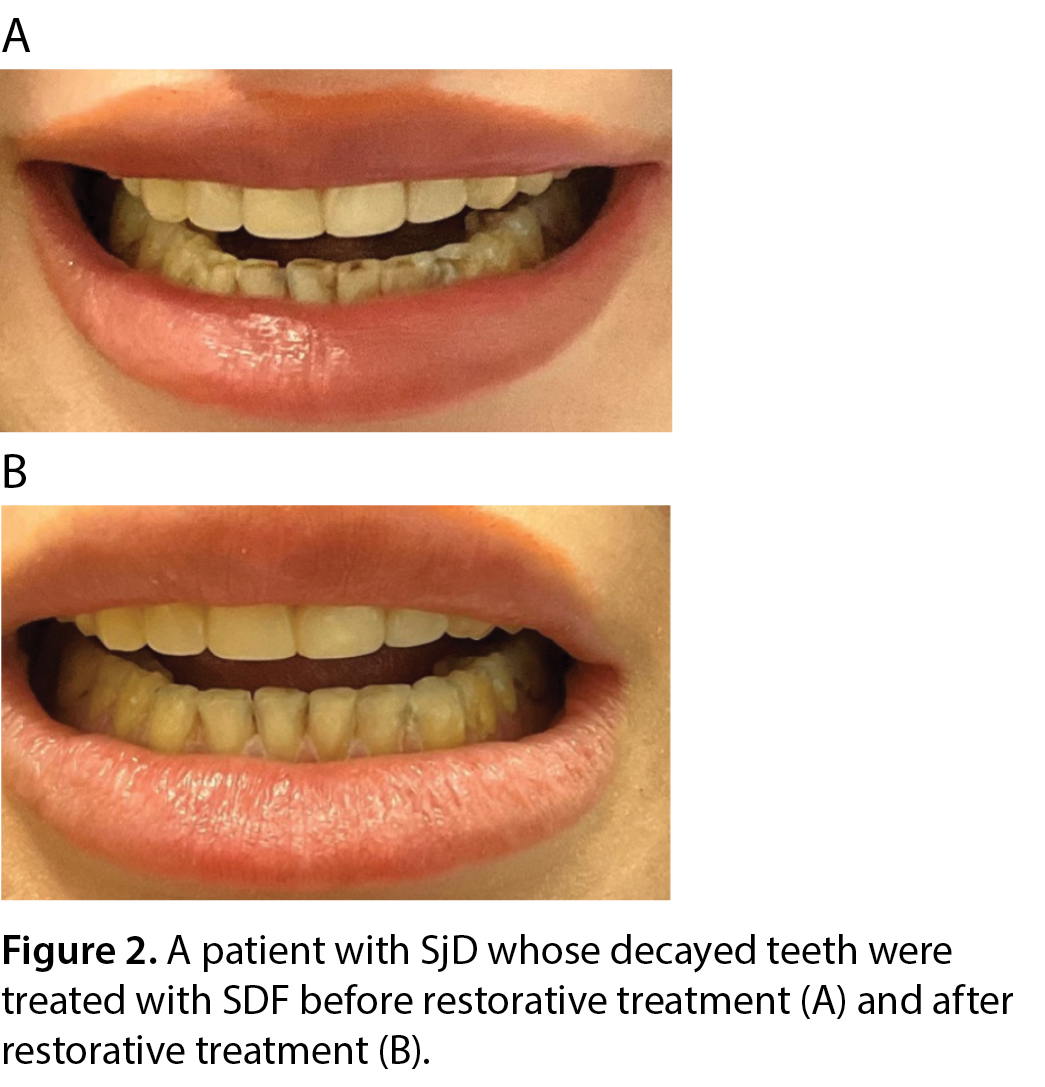
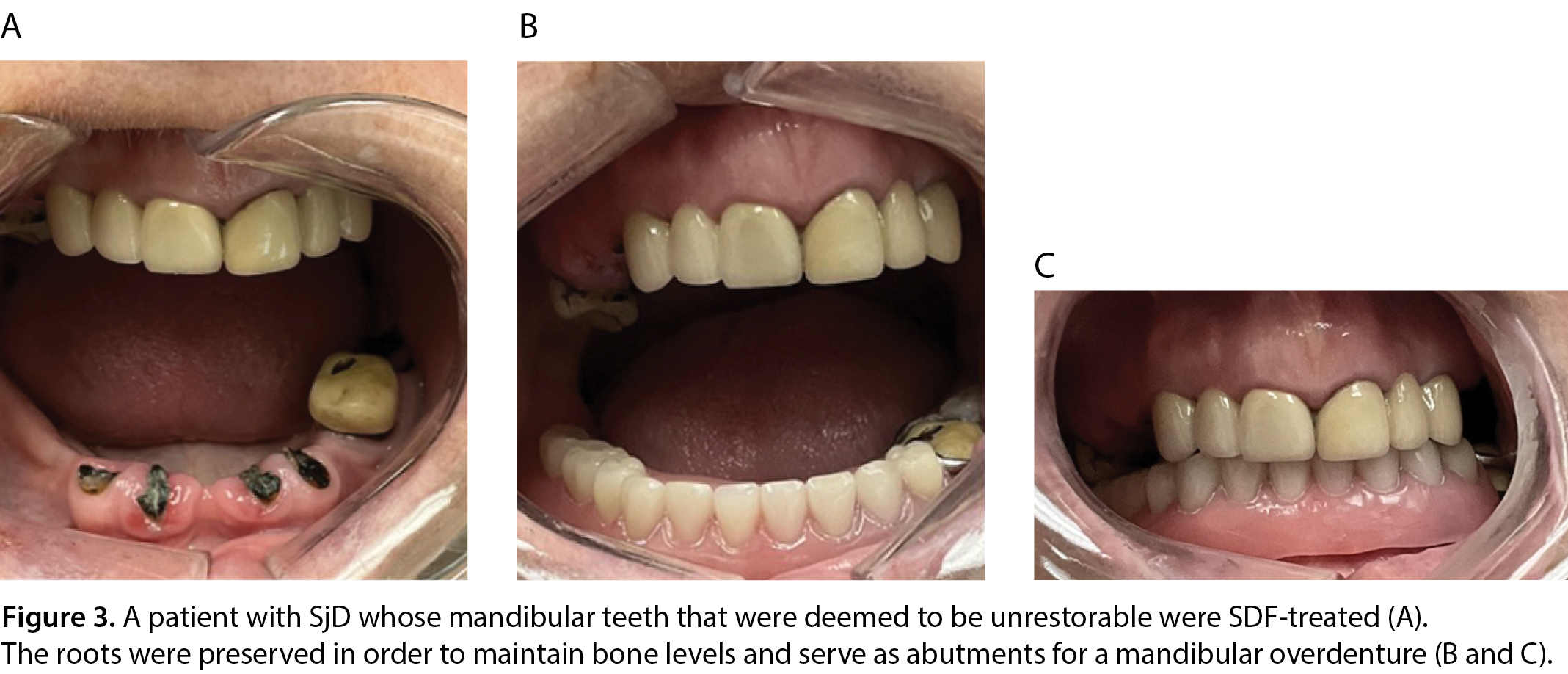
In the event that the mouth has become so dry that rampant caries develop along the gingival margins of teeth through no fault or neglect of the sufferer, e.g., those patients with SjD, there is a treatment regime that has been shown to arrest decay and decrease tooth sensitivity29. The application of SDF by a dentist or hygienist is a minimally invasive treatment for dentine hypersensitivity and carious lesions. It is indicated for use in those patients: with extreme caries risk (e.g., dry mouth or Severe Early Childhood Caries); where treatment is challenged by behavioural or medical management; with carious lesions that may not all be treated in one visit; with difficult to treat dental carious lesions; or without access to dental care30. This treatment in combination with cosmetic bonding (Figure 2) or overdenture fabrication (Figure 3) improves dental aesthetics with minimal invasion and cost, increasing patients’ self-esteem.
Dr. Leslie P. Laing is a clinical associate in the Department of Prosthodontics at the Faculty of Dentistry, University of Toronto; a Prosthodontist and Dry Mouth Specialist at Toronto Public Health Dental and Oral Care Clinics; is in private practices devoted to implant and Prosthodontic dentistry and relief of dry mouth in Toronto, Mississauga, and Brockville, Ontario; and whose roles with the Sjögren’s Society of Canada are: president, co-chair of the Medical Advisory Board; and member of the Board of Directors.
References:
1. Shakespeare, W. The Tragedy of Romeo and Juliet; 1597.
2. Mitchell J. Big Yellow Taxi. Album: Ladies of the Canyon;1970.
3. Mercadante V, Jensen SB, Smith DK, et al. Salivary Gland Hypofunction and/or Xerostomia Induced by Nonsurgical Cancer Therapies: ISOO/MASCC/ASCO Guideline. J Clin Oncol. 2021;39(25):2825-2843. doi: 10.1200/JCO.21.01208. Epub 2021 Jul 20. PMID: 34283635.
4. Trahan L. Xylitol: a review of its action on mutans streptococci and dental plaque – its clinical significance. Int Dent J. 1995; 45(1 Suppl 1):77-92.
5. Tanzer JM. Xylitol chewing gum and dental caries. Int Dent J. 1995; 45(1 Suppl 1):65-76.
6. Hayes C: The effect of non-cariogenic sweeteners on the prevention of dental caries: a review of the evidence. J Dent Educ. 2001; 65(10):1106-1109.
7. Laing LP. Green Tea, Lollipops, Licorice Root: The Sjögren’s Quest. May 2012. Academy of Prosthodontists, Jackson Hole WY.
8. Laing LP. Myths Surrounding Sjögren’s Syndrome. January/February 2019. Ontario Dentist. p:24-27.
9. Ricketts NB. The Mormon Battalion: U.S. Army of the West, 1846-1848. Logan, Utah: Utah State University Press, 1996.
10. Perkins S. History and the Atmosphere. Available at https://www.skysailing.com/hndouts/Essay.pdf. Accessed March 17, 2025.
11. Taylor Hauer S. Available at https://www.moabtimes.com/articles/high-desert-hoofbeatsthe-pits/. Accessed March 17, 2025.
12. Dempsey L. A Little Running Tip: Learning from Native Americans. Life in General, 2019.
13. Pratt H. This Native American Veteran Carried a Pebble into War. American Veteran: Keep it Close. PBS Digital Studios, 2021.
14. Gillespie K, Kodani I, Dickinson DP, et al. Effects of oral consumption of the green tea polyphenol EGCG in a murine model for human Sjogren’s syndrome, an autoimmune disease. Life Sci. 2008;83(17-18). doi:10.1016/j.lfs.2008.08.011
15. Laing LP, Ko J, and James DF. 2011. The Effects of Green Tea on Salivary Flow Production/Flow Rate and Viscosity in Patients with Sjögren's Syndrome: A Pilot Study; International College of Prosthodontists; Hawaii, Big Island, USA.
16. Gabay EL. Flow rate, sodium and potassium concentration in mixed saliva of complete denture-wearers. J Oral Rehabil. 1980 Nov;7(6):435-43. doi: 10.1111/j.1365-2842.1980.tb00462.x. PMID: 693611.
17. Jensen JC, Brodin P, Orstavik J. Parotid salivary flow rates in two patients during immediate denture treatment. J Oral Rehabil. 1991 Mar;18(2):155–62.
18. Yurdukoru B, Terzioglu H, Yilmaz T. Assessment of whole saliva flow rate in denture wearing patients.
J Oral Rehabil. 2001 Jan;28(1):109-12. doi: 10.1046/j.1365-2842.2001.00624.x. PMID: 11298917.
19. Wolff A, Ofer S, Raviv M, et al. The flow rate of whole and submandibular/sublingual gland saliva in patients receiving replacement complete dentures. J Oral Rehabil. 2004 Apr;31(4):340-3. doi: 10.1046/j.1365-2842.2003.01247.x. PMID: 15089939.
20. Matsuda K, Ikebe K, Ogawa T, et al. Increase of salivary flow rate along with improved occlusal force after the replacement of complete dentures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009 Aug;108(2):211-5. doi: 10.1016/j.tripleo.2009.03.020. PMID: 19615661.
21. Tango RN, Arata A, Borges ALS, et al. The Role of New Removable Complete Dentures in Stimulated Salivary Flow and Taste Perception. J Prosthodont. 2018 Apr;27(4):335-339. doi: 10.1111/jopr.12507. Epub 2016 Jul 19. PMID: 27434551.
22. Shanbhag VKL. Oil pulling for maintaining oral hygiene – A review. J Tradit Complement Med. 2017;7(1):106. doi:10.1016/J.JTCME.2016.05.004.
23. Laing LP, Vandersluis Y, Karim JA. September 2017. Sjögren’s Syndrome and Edible Oils: More Than Whistle-Whetting Agents. International College of Prosthodontics. Santiago Chile.
24. Laing LP, Vandersluis Y, Karim JA. April 2018. What’s Old is New Again: Ancient Aryuvedic Oil-Pulling Technique Combats the Microbiome Associated with the Oral Maladies of Sjögren’s Syndrome Patients. 14th International Sjögren’s Syndrome Symposium. Washington DC.
25. Bastin S. and Henken K. Water Amounts in Fruits and Vegetables. Health Matters Program, 2011.
26. Priyanka Tayee AH, Messer R, De Rossi S, et al. Evaluation of pH Values of Products Managing Xerostomia. Dental College of Georgia; Augusta, GA, USA: 2015.
27. Delgado AJ, Olafsson VG, Donovan TE. pH and Erosive Potential of Commonly Used Oral Moisturizers. J Prosthodont. 2016 Jan;25(1):39-43. doi: 10.1111/jopr.12324. Epub 2015 Jul 27. PMID: 26216576.
28. Delgado AJ, Olafsson VG. Acidic oral moisturizers with pH below 6.7 may be harmful to teeth depending on formulation: a short report. Clin Cosmet Investig Dent. 2017 Aug 3;9:81-83. doi: 10.2147/CCIDE.S140254. PMID: 28814900; PMCID: PMC5546593.
29. Laing LP and Karim JA. Use of “Black Magic” in Arresting Oral Decay in Sjögren’s Disease Patients. Oral Health. December 2024: 42-44.
30. Horst JA, Ellenikiotis H, Milgrom PL. UCSF Protocol for Caries Arrest Using Silver Diamine Fluoride: Rationale, Indications and Consent. J Calif Dent Assoc. 2016 Jan;44(1):16-28. PMID: 26897901; PMCID: PMC4778976.
|




