Winter 2024 (Volume 34, Number 4)
Patient-Doctor Perspective
A Journey of Dedication, Resilience
and Triumph
By Muhammad Asim Khan, MD, FRCP, MACP, MACR
Download PDF
I was born in 1944 into an educated middle-class family. However, only three years later, we were forced to relinquish the life we once knew, uprooted from our ancestral lands, never to return. The loss was further deepened by the death of my toddler brother from gastroenteritis. The persistent plight of an ever-increasing number of dispossessed, desperate, and defenseless refugees, mirroring my own fate and faith, continues to weigh heavily on my heart.1
I have suffered from ankylosing spondylitis (AS) since the age of 12, with a diagnosis delayed by six years. Initially, I was under the care of an orthopedist who suspected tuberculosis and treated me with triple therapy: isoniazid, para-aminosalicylic acid, and streptomycin, the antibiotic, which I self-injected intramuscularly every day for a year. When no clinical benefits were observed, he administered intravenous injections of honey, imported from West Germany. That also did not help but it made me ever so sweet, as that honey must still be running in my veins.1
I aspired to excel in my studies and obtained admission to the nation’s oldest and premier medical college at age 16, and ranked first in both anatomy and physiology in the initial examination two years after admission.1 During the start of my clinical rotations, I discussed my symptoms with my professor, who correctly diagnosed my illness and prescribed phenylbutazone, which proved to be very effective.
I graduated in 1965 at 21 years of age, and in September of that year my country was attacked by a neighbouring nation. I voluntarily enlisted in the Army Medical Corps, driven by my zeal to serve the nation that had accepted me as a three-year-old refugee and invested in my education. In my eagerness to serve, I did not reveal my illness.
In 1967, I left the army as a Captain and flew to England for postgraduate training. Two years later, I moved to the United States, where I have had a very fulfilling academic career as a rheumatologist, despite facing many health challenges. I have undergone bilateral total hip arthroplasties and three subsequent surgical revisions. Unfortunately, the very last revision was a disaster, leaving me reliant on a walker and an almost three-inch thick sole on my left shoe.
More than four decades ago, I suffered a neck fracture that failed to heal despite five months of immobilization with a halo device screwed into my skull and attached to a vest encircling my chest. When this method proved unsuccessful, surgical fusion was performed, but I had to continue wearing the halo and the vest for an additional three months. I continued to care for my patients for all of those eight months. Just imagine driving to work and trying to sleep at night leaning back on a chair with that hardware around your head! One day, a new patient came to see me. After our initial handshake, his face turned pale. I immediately had him lie down on the examination table. Once he felt better, he started laughing and said, “Doc, I had been hurting and waiting to see you for two weeks, but with one look at you all my pains are gone!”
I had developed hypertension and coronary artery disease at an early age, and in 1998, I underwent coronary angioplasty with stent placement. The associated anticoagulant therapy caused painless hematuria that led to the discovery of a renal-cell carcinoma for which I underwent radical nephrectomy, and subsequently faced the added uncertainty that a cancer patient has to live with.
More than a decade ago, I was diagnosed with hypothyroidism secondary to pituitary macroadenoma. I consulted several renowned neurosurgeons, but they were reluctant to perform the surgery because of the total immobility of my neck. Determined to proceed, I finally convinced one of them to take the surgical risk by suggesting a pre-operative tracheostomy for intubation to facilitate general anesthesia and provide easier trans-nasopharyngeal access. The surgery was successful although I now require pituitary hormones replacement. Additionally, I have chosen to keep the tracheostomy tube to facilitate any future emergency intubation.
My medical challenges have since expanded to include tophaceous gout, asthma, and severe obstructive sleep apnea, which necessitates the use of a BiPAP machine to sleep. I also wear a cardiac pacemaker. On June 7, 2022, I walked into a hospital at 7:30 am using my
three-wheeled walker and walked out at 7:30 pm the same day with a new aortic valve, without any visible stitches on my body. And two months ago, I underwent a successful coronary artery angioplasty with stent placement in the left anterior descending artery. This "bionic man" is therefore deeply grateful to the Almighty and modern medicine for keeping him going.
I have enjoyed every bit of my life, with all its humor, hardships, hurdles, and dramatic moments that could even appeal to the Hollywood movie moguls.2 I extend my heartfelt gratitude to my family for their unending support.
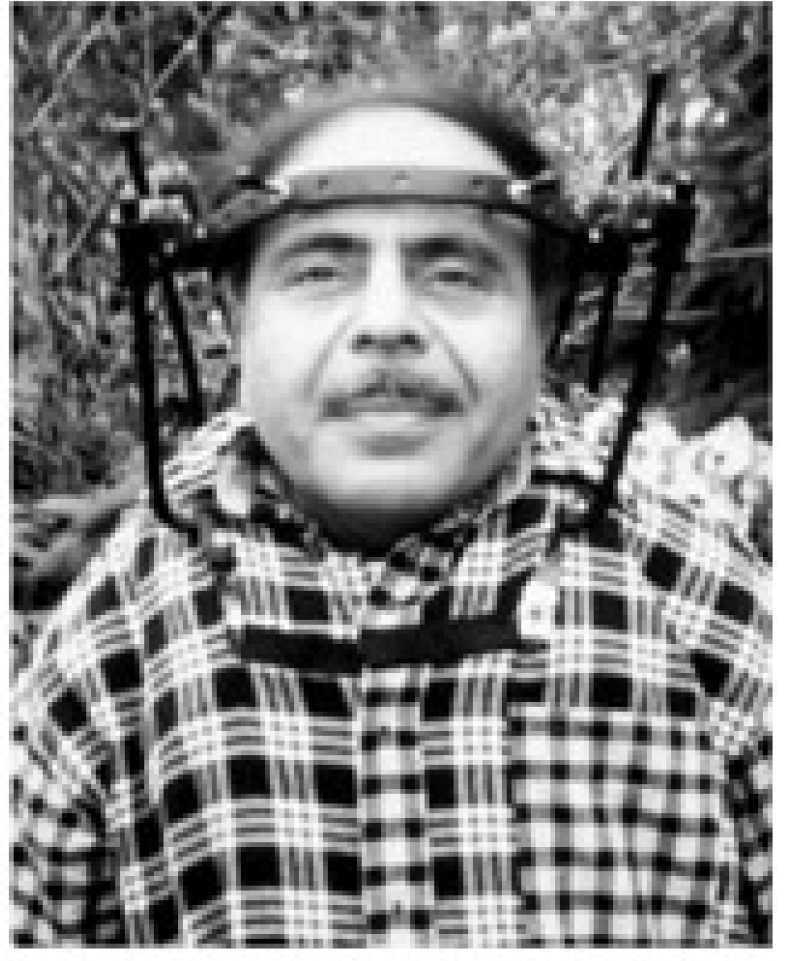
Figure 1. My picture wearing a halo screwed into my skull was taken in 1983. I have republished it with the permission of Blackwell Publishing from MA Khan. Spondyloarthropathies,. In: Hunder G, ed. Atlas of Rheumatology, Oxford, UK, Blackwell Science; 1998:5.1-24.
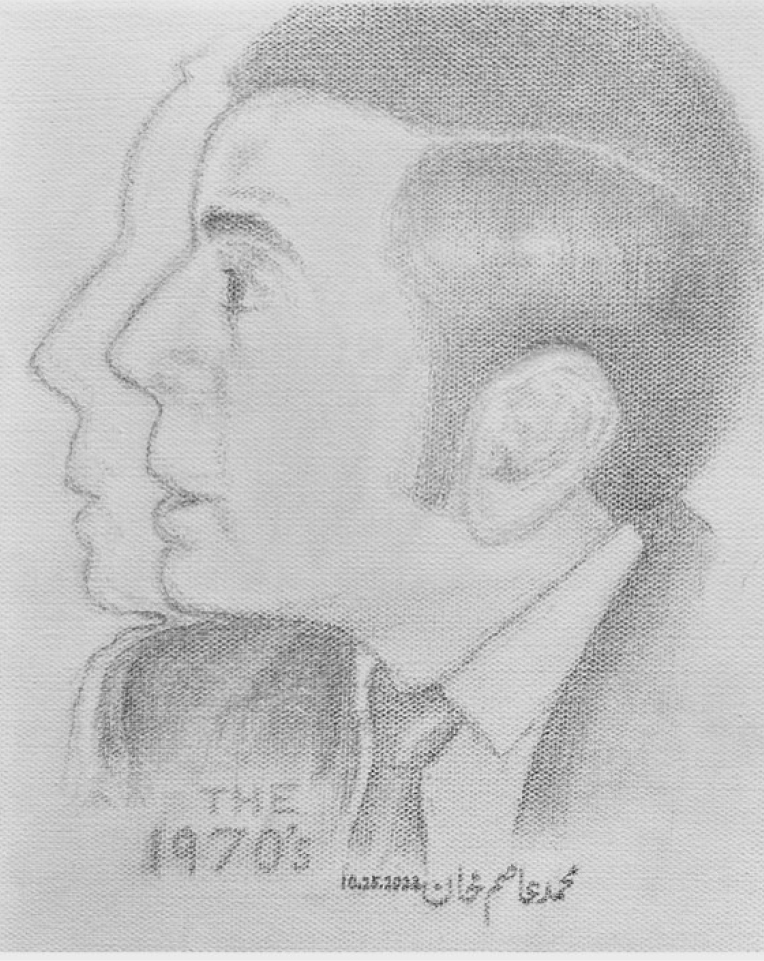
Figure 2. My self portrait drawn with carbon pencils; this is how I looked presenting my scientific abstract at the Annual Scientific meeting of the ARA (now called ACR) in the early 1970s. Please note the long sideburns that were fashionable in those days.

Figure 3. My artistic self-portrait that has been published
(Khan MA. My self-portrait. Clin Rheumatol. 2001; 20:1-2.)
Muhammad Asim Khan, MD, FRCP, MACP, MACR
Professor Emeritus of Medicine,
Case Western Reserve University
Cleveland, Ohio
References:
1. Khan MA. What a life lived despite adversity!. The Kemcolian. 2023; 36 (Spring/Summer): 35-36.
2. Khan MA: Patient-doctor. Ann Intern Med. 2000; 133: 233-235.
|
