Fall 2024 (Volume 34, Number 3)
Mapping the Journey to Rheumatology Team Care in BC (2010-2024)
By Jason Kur, MD, FRCPC
Download PDF
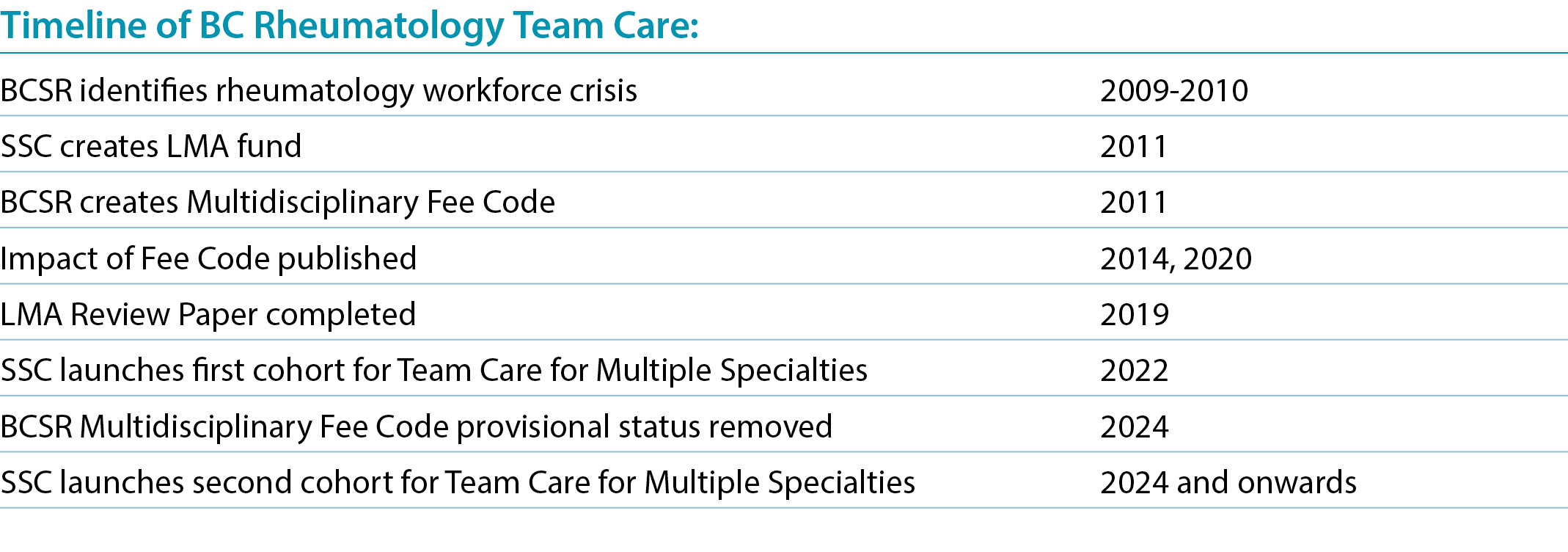
In the early 2000s, rheumatology in British Columbia (BC) was facing a crisis — access to rheumatology care was challenging, there were very few rheumatologists per capita in the province, and the physician workforce was dwindling. The situation was so critical the BC Medical Journal’s cover story, in April 2011, cheekily asked if rheumatologists were an “endangered species”. That stark conclusion came from the work that the BC Society of Rheumatologists (BCSR) undertook to determine the status of the BC rheumatology workforce.
Around the same time, the Specialists Services Committee (SSC), a collaborative committee between the Doctors of BC and the BC Ministry of Health, allocated funding as part of a Labour Market Adjustment (LMA). This funding was agreed to, as part of the 2011 Physician Master Agreement. A 10-million-dollar fund was established for the SSC to distribute to specialities who suffered from the most significant recruitment and retention challenges. I realized it was important for rheumatology to access these funds to help reduce disparity and increase retention.
In my fellowship training at the University of British Columbia (UBC), I was impressed by the collaborative nature of pediatric rheumatology at BC Children’s Hospital. The pediatric rheumatologists worked seamlessly with clinic nurses to help with methotrexate teaching, and these nurses also assisted with patient and parent counselling. At the same time, I also noticed that, in endocrinology, diabetes clinics had the benefit of allied health professionals helping patients manage the complications of chronic disease. At that point, I asked myself, why could/should this not be the case in rheumatology?
On behalf of our section and in dialogue with other rheumatologists, I set about to create a proposal for a change to care delivery in the province. This consisted of several key initiatives, the cornerstone of which was changing the model of care, and the development of a fee code to support the use of nurses in outpatient fee-for-service practice. This code, billable every six months, was characterized as follows: “Multidisciplinary Conference for community-based patients: To consist of assessment, written treatment plan and any other counselling the patient needs for management of their particular diagnosis.”
The other successful changes as part of this process were the creation of (i) a time-based complex care code, as well as (ii) the annual immunosuppressant review checklist for patients on advanced therapies.
The ensuing years saw rheumatologists in BC incorporating nurses in their practices, usually on a part-time basis to assist in the management of patients with inflammatory diseases. It didn’t take long for the BCSR to demonstrate that this model of care had many benefits — including increased access in terms of patient visits, as well as improved provider and patient satisfaction. In addition, the uptake for this model of care was remarkable with 80% of the rheumatologists accessing the fee code. The appetite for system change, even in a traditional fee-for-service model, was evident. Of course, these changes were instigated to improve recruitment and retention. To that end, rheumatology in BC has seen growth in full-time equivalent (FTE) practitioners, with the onboarding of newer physicians now matching with the number of retirements. Moreover, specific studies reflecting on the timeframe (2010-2018) demonstrated that, after the implementation of the LMA codes in 2010, there was an increase in the number of FTE rheumatologists providing outpatient services in BC, rising from 30.0 FTEs in 2010, to 58.4 FTEs in 2018.
Other specialists have taken note of the successes that BC rheumatology has had. Indeed, the SSC has successfully completed a broader project, which supported nine different specialties (medical and surgical), to expand their out-patient specialist team care with the addition of allied health professionals (including nurses, dietitians, and therapists). Drs. Tommy Gerschman and Michelle Teo, both CRA members, led this initial expansion towards a transformative model of team care for specialists in BC. By way of their leadership, a step-by-step toolkit was created to advance specialist success. The first cohort of specialist team care leaders was completed in 2024. The SSC has taken on a second, larger cohort to further build on this success. As the current co-chair of the SSC, it is heartening for me to see this progression of team care gain momentum.
Such a significant change in practice has not surprisingly been associated with some issues along the way. Some of these concerns relate to the time needed to train nurses in rheumatology, finding health care professionals in a limited workforce, office logistics, and even having the clinical space to allow this team model of care to flourish. None of these challenges are insurmountable, but they all need ongoing physician support and attention.
Since the inception of the multidisciplinary team care fee code in BC, years of financial monitoring have occurred. The BCSR has been at the forefront of helping create this sustainable model of care. In 2024 the fee code was finally transferred to the Medical Services Plan general pot and no longer has a provisional code designation. The nursing team model of care has, over the past 14 years in BC, become an established standard of care for patients with inflammatory diseases.
Jason Kur, MD, FRCPC
President, BC Society of Rheumatologists
Co-Chair, BC Specialist Services Committee
Summerland, British Columbia
References:
1. Kur J. and Koehler B. Rheumatologist Demographics in British Columbia: A Looming Crisis. BCMJ 2011; 53(3).
2. Sun M, Jamal S, Kur J. Analysis of Rheumatology Nursing Interventions in Out-patient Practice Settings. CRAJ. 2014; 24,3:18-22.
3. Duncan R, Cheng L, Law MR, et al. The Impact of Introducing Multidisciplinary Care Assessments on Access to Rheumatology Care in British Columbia: An Interrupted Time Series Analysis. BMC Health Serv Res. 2022; 22(1):327.
4. Connell J, Kur J, Gurmin JH. Assessing the Impact of a Nursing Model of Care on Rheumatology Practice Patterns and Patient Satisfaction in British Columbia. BCMJ. 2020; 62(3):98-102.
5. Specialist Services Committee. “Consultant Specialist Team Care Toolkit”. May 2024. Available at https://sscbc.ca/sites/default/files/DoBC%20CSTC%20Toolkit%20V3.pdf. Accessed September 2, 2024.
|




