Summer 2022 (Volume 32, Number 2)
The CRA's 2022 Distinguished
Rheumatologist:
Dr. John G. Hanly
Download PDF

Why did you become a
rheumatologist? What or who
influenced you along the way to do so?
My reasons for deciding to become a
rheumatologist are in large part due
to the influence of Professor Barry
Bresnihan, with whom I worked for two
years (1982-1984) in Dublin, Ireland.
He was my role model, and his mentorship
has sustained me throughout
my career. Steadfast in his commitment
to advancing care for patients
with rheumatic diseases through research,
he overcame significant professional
challenges in his own career.
Moreover, he inspired a cadre
of rheumatology fellows to pursue an
academic career track and most went
on to establish independent research
programs in Ireland or abroad. On a personal note, he was
also great fun to be with and treated me as an equal despite
the gap in seniority.
Born in Ireland and having obtained your medical degree
from the National University of Ireland in 1978, you began
your medical career in Dublin where you pursued a two-year
Rheumatology Research Fellowship with Professor
Barry Bresnihan in Dublin. This was focused on the clinical
efficacy and immunomodulatory effects of total lymphoid
irradiation in patients with severe rheumatoid arthritis.
In 1984, you emigrated to Canada and undertook clinical
fellowships in rheumatology and immunology at the
University of Toronto and McMaster University.
a) From where did your passion and interest for
rheumatology stem?
There are many attractive features to our specialty, both
from a clinical and scientific perspective. These include
the diversity in the types and severity of clinical disease,
the opportunity to link basic science observations to the
patient and the eventual translation of basic science to
meaningful therapies, as a few examples.
b) Can you tell us more about your professional journey
from Ireland to Canada and why you made the decision to
move to Canada?
When I left Ireland in 1984 it was customary to pursue
subspecialty training outside the country, either in the UK
or in North America. My twin brother,
who is a respirologist, had relocated
to Canada a couple of years earlier,
so that was one reason. The other was
that there were opportunities for both
my wife (also a physician) and me, in
Canada, at McMaster University and
the University of Toronto, respectively.
In addition to your clinical and
teaching activities you are also a
respected clinical investigator. As
a researcher you have received
continuous peer-reviewed funding
from the Canadian Institutes of
Health Research (CIHR) since 2002.
Your focus has been the study of
pathogenic mechanisms of systemic
lupus erythematosus and their
clinical outcomes. Your most significant contributions
have related to the effects of lupus on the brain and other
parts of the nervous system. Your publication record on
neuropsychiatric lupus is internationally recognized. Can
you tell us more about your research and its impact on our
understanding of SLE and its implications for patients?
My decision to focus on nervous system lupus in the early
part of my career was somewhat fortuitous and assisted
by the support of colleagues during my training and at
my home institution in Halifax. Early work contributed
to our understanding of pathogenetic mechanisms and
the clinical course of cognitive dysfunction, one of the
most common forms of nervous system lupus. In the last
20 years I have been able to extend this work to a large,
international inception cohort of SLE patients. This effort
has received long-term funding from CIHR, resulted in
several high-profile publications and fostered many collaborations
with colleagues across Canada and the world.
The messages for patients are that only 30% of all nervous
system events in SLE patients are attributable to lupus, the
outcome of these events is frequently very good, and we are
steadily advancing our understanding of how lupus affects
the brain and other parts of the nervous system.
On an international level, you are Past Chair of the Systemic
Lupus International Collaborating Clinics (SLICC), an
international research network of lupus investigators in 16
countries. Through your ongoing membership of national
and international networks involved in clinical studies of lupus, you continue to be a productive contributor to this
field. How has international collaboration helped shape
the field of rheumatology, and specifically SLE, here and
elsewhere?
SLE is a relatively rare disease, so collaborative research
is important to achieve success. The Canadian centers involved
in SLICC have contributed substantially through
leadership of the organization, championing individual research
projects and patient recruitment. Over the past 30
years the collective success of SLICC has greatly exceeded
what any individual SLICC center could have achieved in
isolation. Knowledge gained has been translated to improvements
in SLE patient care.
What is the greatest professional and organizational
challenge you have faced, and how did you address/
overcome this challenge?
All clinician researchers are challenged to protect their
time for research while fulfilling their other clinical and
academic responsibilities. The goodwill of local colleagues,
a supportive academic environment and a steadfast
belief and commitment to the mission are key to success.
What major changes to the landscape of rheumatology
have you witnessed over the course of your career?
The emergence of new diagnostic and therapeutic modalities
in the advancement of clinical care, and the value
of research collaboration as a key component to scientific
advancement and success.
What do you foresee as challenges to Canadian
rheumatologists in the future and what can individual
rheumatologists and the CRA do to meet these challenges?
In clinical practice, the administrative burden involved in
securing access to new medications for patients is ever
increasing. Clinician-researcher positions in academic
rheumatology centers have not kept pace with expanding
rheumatology resources and “hard” funding for such
positions is diminishing. The CRA is the profession’s
advocate to address both issues.
You are the recipient of numerous awards in recognition
of your achievements in lupus research, including the ACR
Edmund L. Dubois Memorial Award, the CRA Distinguished
Investigator Award and the Ira Goldstein Honoree Award
from New York University. Furthermore, you have also been
designated a Master by both the CRA and ACR. What was
your first thought when you learned that you would be
receiving the CRA Distinguished Rheumatologist Award?
I was flattered, grateful and humbled to receive the award.
It was an honour to join the list of outstanding rheumatologists
who had previously received the award.
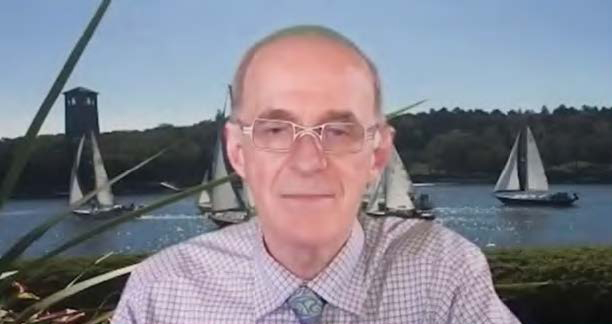
Dr. Hanly receiving the CRA Distinguished Rheumatologist
Award during
the virtual gala in February 2022.
What do you believe are the qualities of a distinguished
rheumatologist?
I hope that the designation would apply to one who has
contributed to advancing the care of patients with rheumatic
diseases.
What is your favourite food or cuisine?
My wife’s!
What are your dream vacation destinations?
Safari in Kenya and visiting New Zealand.
How many cups of coffee does it take to make a productive
day?
Two
We understand you have an identical twin who is also a
distinguished physician, now in Canada. How were your
career paths intertwined and how did you help each other
to achieve professional success?
The bond between identical twins is special and probably
unique among siblings. My brother and I have both pursued
an academic career track in medicine, albeit in different
specialties. We have had shared experiences navigating
this route and been able to advise each other at different
junctures — be that in the academic or political spheres.
We are both married to wonderful and inspiring spouses
who are also academic physicians and have enjoyed great
success in their own careers. My brother and I continue
to share similar interests outside of work — gardening,
fly fishing and rugby (enduring life-long supporters of
Munster Rugby and Ireland).
John G. Hanly, MD, FRCPC
Professor of Medicine and Pathology,
Research Director, Division of Rheumatology
Department of Medicine,
Dalhousie University and
Queen Elizabeth II Health Sciences Center,
Halifax, Nova Scotia
|
