Spring 2022 (Volume 32, Number 1)
Incidence of the SARS-CoV-2 Infection
Amongst Patients with Rheumatological
Conditions:
A Single Centre Study
By Amirsadegh Yazdani; and Ramin Yazdani, MD, MRCP (UK), FRCPC
Download PDF
The SARS-CoV-2 pandemic has affected the lives of
many individuals, directly or indirectly. Patients
with rheumatological conditions have felt the effects
of the pandemic more so than healthy individuals,
either due to their assumptions of being immunosuppressed,
either because of their underlying conditions
or their treatments. This fear may lead to the discontinuation
of their treatments, avoidance of doing their
drug monitoring tests, or failure to attend their appointments.
To assess the effects of the pandemic on rheumatological
patients, multiple efforts have been undertaken. The
greatest one is the Global Rheumatology Alliance, in which
any rheumatologist can register their patients who have
been affected by the SARS-Cov-2 infection.1
Several factors have been reported to be associated with
the worst outcomes regarding SARS-CoV-2 infection, including
systemic lupus erythematosus (SLE), high disease
activity, high-dose steroids, rituximab, abatacept, and JAK
inhibitors.2
However, presenting local data to patients might have
more impact in alleviating patients’ concerns, and providing
them with the answers they seek. We present the individuals
who have been affected by SARS-CoV-2 infection
in a community rheumatology center in Ottawa, Canada,
between March 2020 and October 2021.
The number of patient visits between March 2020
and October 2021 was about 4,800 (virtual and inperson).
Infections were self-reported by the patients during
their consultations. Thirty-one individuals were affected
by the SARS-CoV-2 infection, nine of whom were males
and 22 were females. The age of these patients ranged from
25-86 years, with a median age of 58 years. The BMI of
patients ranged from 19-51 with a median BMI of 30.75.
Nine individuals were born outside of Canada. Thirty individuals
had an autoimmune rheumatic condition. One
had gout and metabolic syndrome. Twenty-seven individuals
were taking either conventional disease-modifying
antirheumatic drugs (csDMARDs), or biologic DMARDs,
or both (see Table). Six patients were hospitalized due to
the SARS-CoV-2 infection and were treated according to
local guidelines. Only one patient died due to SARS-CoV-2
infection. She was 86 years old with gout, diabetes mellitus,
hypertension, stage 3 chronic kidney disease (CKD3),
and had a BMI of 43 (she was not on DMARDs or biologics).
In our centre, we did not observe increased mortality
in rheumatological patients who are taking csDMARDs or
bDMARDs.
The following table summarizes the
patients’ characteristics and outcomes.
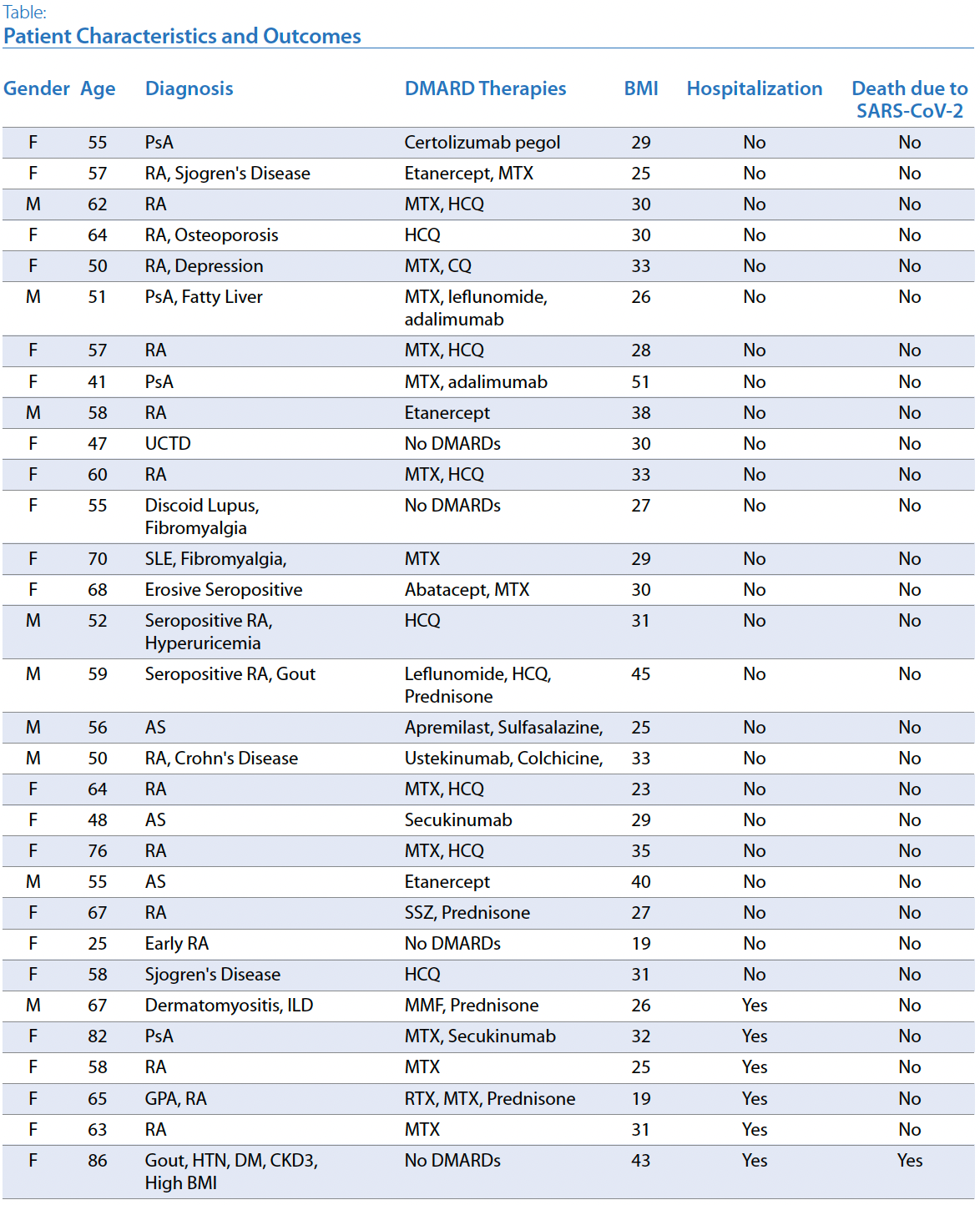
PsA, psoriatic arthritis; RA, rheumatoid arthritis; MTX, methotrexate, HCQ, hydroxychloroquine; CQ, chloroquine; UCTD, undifferentiated
connective tissue disease; DMARDs, disease-modifying antirheumatic drugs; SLE, systemic lupus erythematosus; AS, ankylosing spondylitis,
SSZ, sulfasalazine; MMF, mycophenolate mofetil; ILD, interstitial lung disease; GPA, granulomatosis with polyangiitis; RTX, radiotherapy;
HTN, hypertension; DM, diabetes mellitus; CKD3, stage 3 chronic kidney disease; BMI, body mass index
Amirsadegh Yazdani
Student,
Ottawa, Ontario
Ramin Yazdani, MD, MRCP (UK), FRCPC
Rheumatologist,
Ottawa, Ontario
References:
1. Covid-19 Global Rheumatology Alliance. Available at rheum-covid.org. Accessed February 6, 2022.
2. RheumNow. Available at rheumnow.com. Accessed February 6, 2022.
|




