Spring 2022 (Volume 32, Number 1)
Characterization of the
Rheumatologist-Extended Role
Practitioner Model of Care in an
Inpatient Tertiary Care Network
Lena Nguyen; Marie-Andree Brosseau, PT; Nancy Granger, MScPT, MSc; Julia Ma, MPH;
Andrew Chow, MD, FRCPC; and Stephanie Tom, MD, FRCPC
Download PDF
Introduction:
Models of care (MOC) have become crucial to address
rheumatologist workforce shortages and increasingly complex
patient needs. In Canada, leveraging the involvement
of extended role practitioners (ERP) in outpatient rheumatology
settings has been shown to decrease wait times.1-2
The first Canadian rheumatologist (MD)-ERP MOC for
inpatients was introduced at Trillium Health Partners
(THP) in 2015. Our ERPs are physiotherapists who completed
the Advanced Clinician Practitioner in Arthritis
Care (ACPAC) program.
Methods:
We undertook a retrospective, cross-sectional chart review
of all patients referred to the rheumatology inpatient
consultation service at THP, which includes the Mississauga
Hospital (MH) and Credit Valley Hospital (CVH)
sites, to characterize the modern inpatient rheumatology
consultation service where they were assessed by the ERPMD
team from January 1, 2015 to December 31, 2019. A
retrospective chart review was conducted using the hospital’s
electronic medical records system and descriptive
analyses performed.
Results:
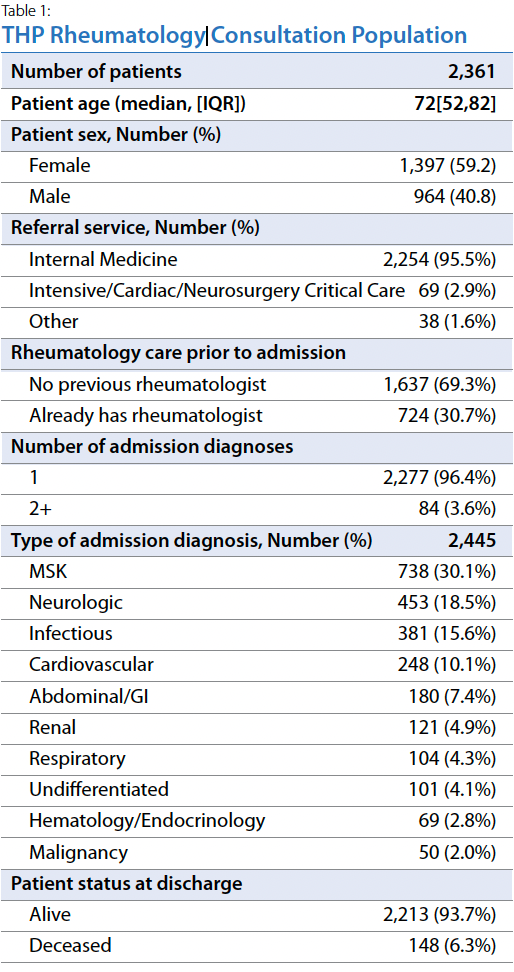
A total of 2,361 patients were seen by the MD-ERP team
between January 2015 and December 2019. The overall
cohort had a median age of 72 and included more females
(59%) than males (41%). The majority of rheumatology
referrals (96%) came from wards (hospitalist, internal
medicine, surgery); only a few were from intensive care
or coronary care units (3%). Most consults were new patients
with no prior rheumatology contact (69%). The
most common reason for hospitalization was a musculoskeletal
(MSK) diagnosis (30%), which included possible
rheumatologic or orthopedic etiology, followed by neurologic
(19%) and infectious (16%) admission diagnoses
(Table 1).
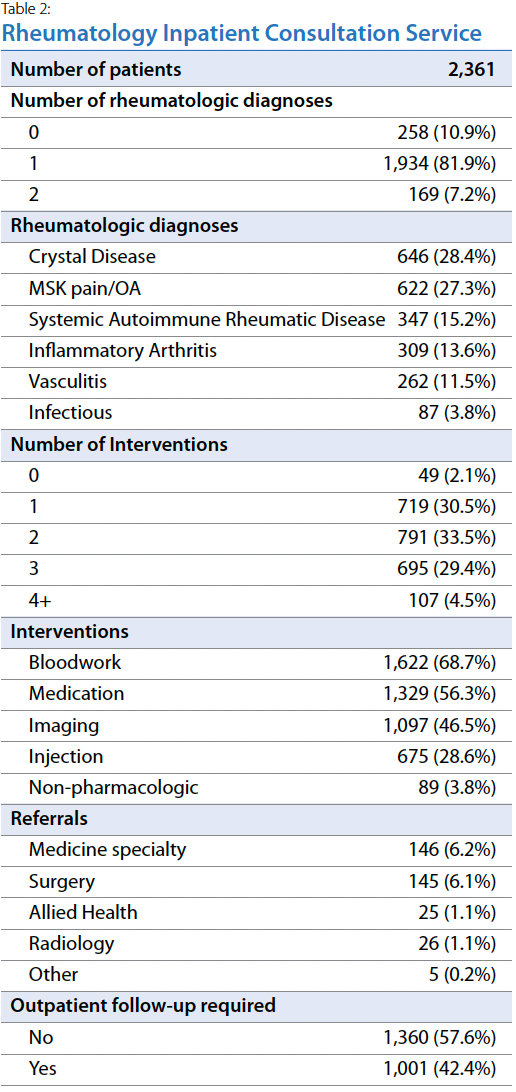
The most common rheumatologic diagnoses were crystal
disease (28%) followed by osteoarthritis (OA)/MSK-related
pain (27%). Less common were systemic autoimmune
rheumatic diseases (15%), inflammatory arthritis
(14%), vasculitis (12%), and infection (4%). Of the 169
patients with concurrent diagnoses, the most common
concomitant diagnoses were crystal disease and OA/MSK-related
pain (50%). Nearly all rheumatology consultations
required interventions (98%), which included bloodwork
(69%), medication (56%), imaging (47%), and/or intraarticular
injection (29%), with most requiring more than
one intervention (Table 2).
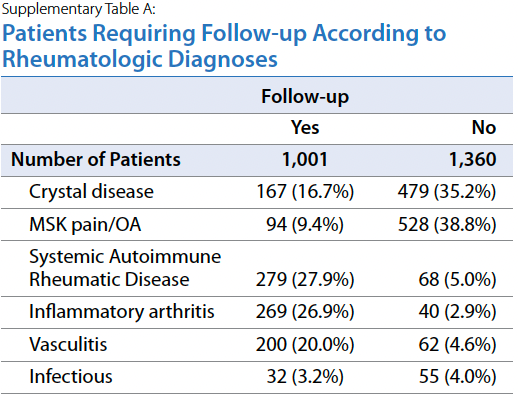
Of all the consulted patients, 42% required outpatient
follow-up (Table 2), particularly those with systemic autoimmune
rheumatic disease (28%), inflammatory arthritis
(27%), and vasculitis (20%) (Supplementary Table A).
Discussion:
With the goals of addressing unmet inpatient needs and
sustainability of hospital-affiliated community practice,
THP implemented the first Canadian inpatient MD-ERP
MOC. Most patients had no previous contact with rheumatology
and only required intervention during their hospitalization.
The most common rheumatologic diagnoses
were crystal disease and OA/MSK-related pain which corresponds
to their prevalence in the general population.3
Although it is important to have rheumatologic management
in high acuity inpatient situations (i.e. life-threatening
vasculitis), the modern rheumatology service
also includes OA/MSK-related pain and crystal disease management.
Crystal disease was the most common rheumatologic
diagnosis, an observation that aligns with studies
reporting gout and pseudogout as the main causes of hospitalizations
related to crystal arthropathies.4-6 Notably,
several studies draw links between deficits in pre-hospital
care7-9 and lack of urate-lowering therapy among hospitalized
patients.10-12 OA was another common reason
for rheumatologic consultation likely due to comorbidity
(i.e. the impact of OA on gait safety and discharge planning).
Due to many rheumatologists’ practice scope being
focused on inflammatory conditions to cope with human
resource shortages.13 OA/MSK-related issues and crystal
disease are typically managed by primary care providers
pre-and post-admission.
Conclusion:
With the increasing burden of rheumatic diseases and too
few rheumatologists, ERPs are integral to supporting inpatient
rheumatology care. Our study provides a benchmark
for future implementations of similar MOCs and highlights
an opportunity to improve outpatient management of
chronic conditions to mitigate future disease burden. More
research is required to evaluate the economic impact of
rheumatology consultation and inpatient MD-ERP MOC.
Acknowledgements:
Thank you to our patients, their families, and their healthcare
provider teams for making this study possible and to
Dr. Judith Versloot for her expertise and input on research analysis.
Declaration of Interest Statement:
The authors declare that they have no known competing financial
interests or personal relationships that could have
appeared to influence the work reported in this paper. This
research was completed for quality improvement purposes
to evaluate our current MOC.
Lena Nguyen
Medical student,
Faculty of Medicine
University of Toronto
Toronto, Ontario
Marie-Andree Brosseau, PT
Advanced Practice Physiotherapist,
Trillium Health Partners
Mississauga, Ontario
Nancy Granger, MScPT, MSc
Advanced Practice Physiotherapist,
Trillium Health Partners
Mississauga, Ontario
Julia Ma, MPH
Biostatistician,
Institute for Better Health
Trillium Health Partners
Mississauga, Ontario
Andrew Chow, MD, FRCPC
Rheumatologist,
Trillium Health Partners
Mississauga, Ontario
Lecturer, University of Toronto
Associate Professor, McMaster University
Hamilton, Ontario
Stephanie Tom, MD, FRCPC
Division Head, Rheumatology
Trillium Health Partners
Mississauga, Ontario
Lecturer, University of Toronto,
Toronto, Ontario
References:
1. Ahluwalia V, Lineker S, Sweezie R, Bell MJ, Kendzerska T, Widdifield J, Bombardier C, Allied Health
Rheumatology Triage Investigators. The effect of triage assessments on identifying inflammatory
arthritis and reducing rheumatology wait times in Ontario. The Journal of Rheumatology. 2020;
47(3):461-7.
2. Passalent L, Hawke C, Lawson DO, et al. Advancing early identification of axial spondyloarthritis:
an interobserver comparison of extended role practitioners and rheumatologists. The Journal of
Rheumatology. 2020; 47(4):524-30.
3. Vos T, Lim SS, Abbafati C, et al. Global burden of 369 diseases and injuries in 204 countries and
territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The
Lancet. 2020; 396(10258):1204-22.
4. Zleik N, Elfishawi MM, Kvrgic Z, et al. Hospitalization increases the risk of acute arthritic flares in gout:
a population-based study over 2 decades. The Journal of Rheumatology. 2018; 45(8):1188-91.
5. Villion A, Arinzon Z, Feldman J, et al. Crystal-Induced Arthropathy in Elderly Patients Hospitalized for
Acute Conditions. The Israel Medical Association Journal: IMAJ. 2017; 19(3):183-5.
6. Lim SY, Lu N, Oza A, et al. Trends in gout and rheumatoid arthritis hospitalizations in the United
States, 1993-2011. JAMA. 2016; 315(21):2345-7.
7. Kuo CF, Grainge MJ, Mallen C, et al. Rising burden of gout in the UK but continuing suboptimal
management: a nationwide population study. Annals of the rheumatic diseases. 2015; 74(4):661-7.
8. Neogi T, Hunter DJ, Chaisson CE, et al. Frequency and predictors of inappropriate management of
recurrent gout attacks in a longitudinal study. The Journal of Rheumatology. 2006; 33(1):104-9.
9. Singh JA, Hodges JS, Toscano JP, et al. Quality of care for gout in the US needs improvement. Arthritis
Care & Research: Official Journal of the American College of Rheumatology. 2007; 57(5):822-829.
10. Wright S, Chapman PT, Frampton C, et al. Management of gout in a hospital setting: a lost opportunity.
The Journal of rheumatology. 2017; 44(10):1493-8.
11. Nitichaikulvatana P, Upchurch KS, Harrold LR. The Impact of Deficits in Gout Care on Hospitalizations.
Journal of clinical rheumatology: practical reports on rheumatic & musculoskeletal diseases.
2011; 17(7):389.
12. Hutton I, Gamble G, Gow P, et al. Factors associated with recurrent hospital admissions for gout: a
case-control study. JCR: Journal of Clinical Rheumatology. 2009; 15(6):271-4.
13. Barber CE, Jewett L, Badley EM, et al. Stand up and be counted: measuring and mapping the
rheumatology workforce in Canada. The Journal of Rheumatology. 2017; 44(2):248-57.
|
