Fall 2022 (Volume 32, Number 3)
Still’s Got That Fever: Adult-onset Still’s
Disease in Fever of Unknown Origin
By Ming K. Li, BHSc; Calandra Li, MSc; Anas Makhzoum, MD; and Rohan Philip, MD
Download PDF
Abstract:Still’s Got That Fever is a case report of a patient in her 60s, who presented with a 2-week history of
fevers, diffuse arthralgias, and salmon-coloured rash. Given the rarity of this disease, it was almost 1 week into
her admission before the diagnosis of adult-onset Still’s Disease (AOSD) was made as the cause of her fever of
unknown origin. This case highlights the Yamaguchi criteria, which are still the standard in making the diagnosis,
which is a clinical one. Our patient underwent extensive investigations to rule out other infectious, malignant, and
auto-immune causes. Furthermore, a life-threatening complication of AOSD that clinicians should be aware of is
macrophage activation syndrome (MAS). The gold standard investigation to rule out MAS is bone marrow biopsy,
which would show hemophagocytosis. Our patient did not develop MAS, was treated with steroids, and showed
an immediate clinical response. We highlight other treatment options for AOSD based on disease severity, including
methotrexate and biologics.
Key Points:
-
Adult-onset Still’s Disease (AOSD) is a rare inflammatory disease that is diagnosed clinically, with
symptoms including high fevers, arthralgias, and a maculopapular rash.
- Investigations should include an infectious and inflammatory work-up, which typically shows an elevated
ESR,a CRP,b and ferritin, but negative blood cultures, ANA,c and RF.d
- An important life-threatening complication rarely associated with AOSD is macrophage activation
syndrome (MAS). It also presents with high fevers, high ferritin, and abnormal liver enzymes, but can
progress to profound cytopenias and liver dysfunction. A bone marrow biopsy is the gold standard to
rule out MAS.
- Steroids are the mainstay of treatment in patients with moderate disease (usually 0.5-1 mg/kg/day);
however, pulse steroids, methotrexate, and biologic therapies may be considered for more severe-to-resistant
disease.
|
Case Presentation:
|
A 64-year-old otherwise-healthy female presented with a 2-week history of recurrent fevers (max temperature
40.0°C), chills, bilateral otalgia, sore throat, generalized rash, migratory arthralgias and myalgias, and non-bloody
diarrhea. Her exam on admission was pertinent for fever (38.8°C), 0.5 cm tender, mobile anterior cervical lymph
nodes, and patches of pruritic rashes over the anterior trunk, and both thighs and arms. Over time, her ear
pains and sore throat resolved, but she continued to have daily self-resolving fevers, arthralgias, and developed a
salmon-coloured rash.
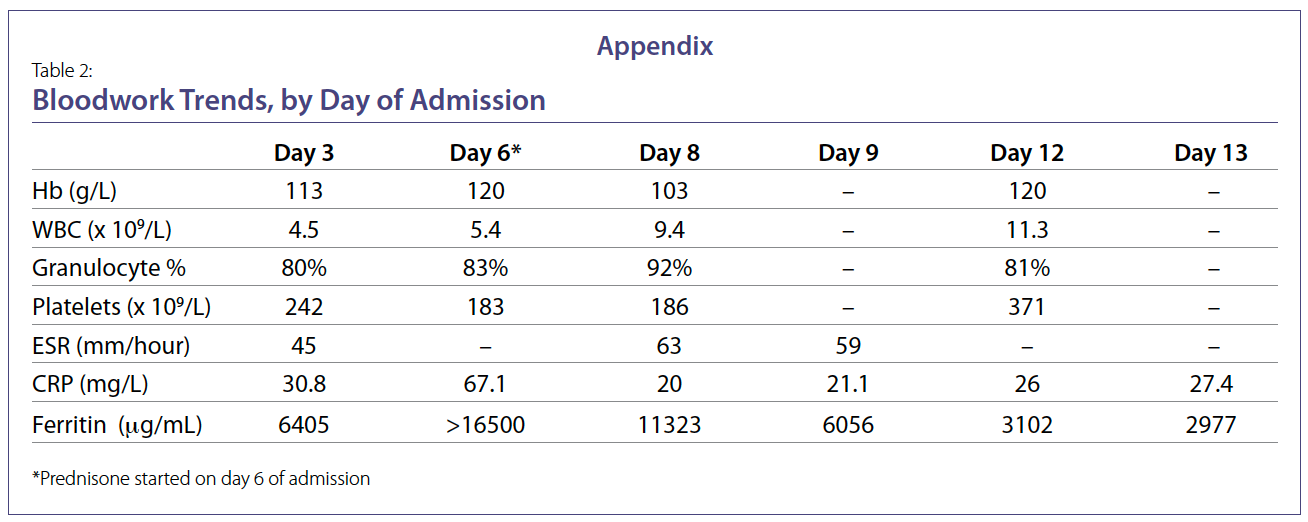
Her investigations revealed elevated ferritin, ESR, and CRP on day 5 of admission, with imaging evidence of
inflammatory arthritis of the wrists, elbows, and knees. Her infectious work-up, including pan-cultures and
CT,e revealed no source of infection, and her rheumatologic panel (ANA, ENA,f ANCAs,g rheumatoid factor,
anti-CCP,h complement studies) were all normal. A bone marrow biopsy was normal. Clinically, she was diagnosed
with Still’s Disease, and was started on prednisone, which resulted in improvement of her symptoms
and inflammatory markers. She was discharged in stable condition on prednisone with outpatient rheumatology
follow-up. At her 8-week follow-up, her symptoms remained well-controlled and methotrexate was
added as a steroid-sparing agent. |
Clinical Manifestations
Patients with adult-onset Still’s Disease (AOSD) present
with a constellation of symptoms, the most common being
severe arthralgias/arthritis, fevers, and subacute rashes.1
It is a rare disease with an incidence of 1/625,000.2 As
seen with our patient, in about 70% of cases, patients present
with a prodromal sore throat prior to manifestation
of AOSD symptoms.3 There is a bimodal age distribution
(peaks between 15-25 and 36-46), although our patient
was asymptomatic until her 60s, which is a late presentation
compared to typical ages of onset.1
Fevers in AOSD are usually quotidian, >39°C, with
self-resolution within 2-4 hours.4 A minority of patients
(<20%) have double-quotidian fevers with a second fever
spike during the day.4 Patients tend to feel quite unwell during
these febrile spikes. Given these fevers, many patients
undergo a work-up for infectious causes which come back
negative, and do not respond to antibiotics.
The joint involvement in AOSD may initially start with
one or few joints, then most commonly progresses to become
polyarticular, affecting both small and large joints.5
Arthrocentesis usually reveals inflammatory arthritis.
Our patient presented with bilateral knee, wrist, and elbow
arthralgias. An arthrocentesis was not pursued given
her improvement with steroids and our level of diagnostic
certainty.
Rash in AOSD is very common, characteristically described
as a salmon-coloured, non-pruritic rash usually
present on the trunk, arms, or legs.5 In some patients, this
rash is only present during fevers.4 Our patient indeed had
a salmon-coloured rash, but it was quite pruritic, requiring
potent topical lotions, and persisting during afebrile
periods.
Diagnosis
AOSD is primarily a clinical diagnosis, and a broad differential
should always be considered, given the non-specific
constellation of symptoms. There is no investigation that
confirms AOSD, but the clinical presentation and laboratory
findings should be used in conjunction to make the
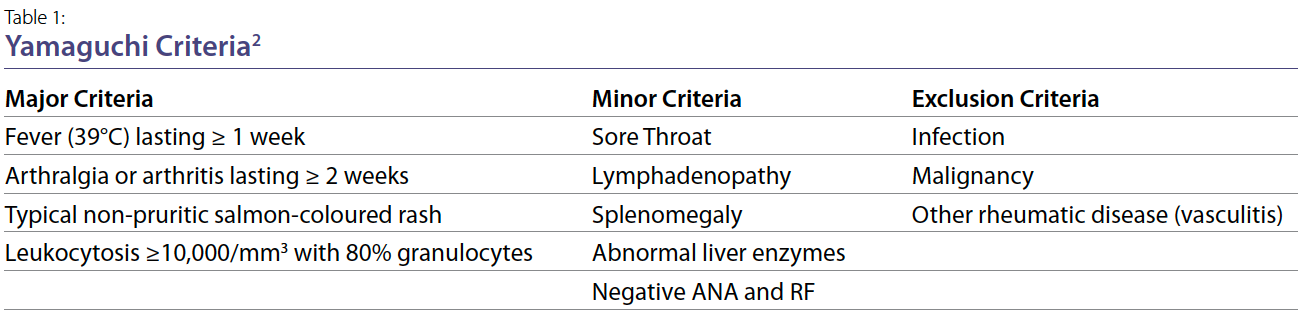
diagnosis. It is usually a diagnosis of exclusion. The Yamaguchi
criteria, first described in 1992, have a sensitivity
of 96.2% and specificity of 92.1%.2 A diagnosis of AOSD
requires ≥5 criteria (≥2 major criteria) and no exclusion
criteria. The criteria are shown in Table 1, with major criteria
including fever ≥1 week, arthralgias ≥2 weeks, typical
non-pruritic rash, and leukocytosis ≥10,000/mm3.2 Our
patient met 3 major criteria and 3 minor criteria.
When suspecting AOSD, important investigations include
CBC,i liver enzymes, ESR, CRP, ferritin, ANA, and RF.4
An infectious work-up including pan-cultures should be
conducted to rule out infectious diseases. As evidenced by
our patient, patients commonly will have elevated leukocyte
count, ferritin, ESR, and C-RP, but negative ANA and
RF. There was no clinical evidence of any other rheumatological
disease. Finally, her pan-CT showed no evidence of
malignancy. Thus, she did not meet any of the exclusion
criteria.
AOSD is typically not a life-threatening disease; however,
a rare life-threatening complication of which physicians
should be cognizant is macrophage activation syndrome
(MAS). Such patients will have high fevers, elevated
ferritin, and abnormal liver enzymes, and can deteriorate
quickly. A bone marrow biopsy would show hemophagocytosis,
and should be strongly considered, to rule out this
life-threatening complication.4 Our patient’s biopsy was
normal.
Treatment
Given that AOSD is quite rare, treatment is extrapolated
from other autoimmune conditions such as rheumatoid
arthritis and SLE. AOSD management depends on disease
severity, with steroids being the mainstay of treatment.6
As there is no well-validated prognostication tool available
for AOSD, treatment goals are targeted to control
inflammatory signs, symptoms, and laboratory indices.4
Mild-to-moderate disease, defined by non-disabling symptoms,
may be initially treated with NSAIDsj and glucocorticoids.
Depending on severity and individual patient assessment,
initial doses of glucocorticoids, like prednisone,
can range from 0.5 mg/kg/day to 1 mg/kg/day.
Moderate-to-severe disease, characterized by persistent
debilitating symptoms, may require addition of a biologic
agent, like anakinra, or other interleukin-1 inhibitors. Anakinra
has shown efficacy as a monotherapy in early disease
and in prevention of chronic arthritis and inflammation later on.7 At this stage, combination therapy with glucocorticoids
may be needed for symptom control. Furthermore,
DMARDs,k such as methotrexate, may be initiated after
2 weeks of symptom non-resolution, or as steroid-tapering
adjuncts long-term. Methotrexate can be used for
3-6 months after discontinuing steroids.
Conclusion
Given its rarity and non-specific symptoms, AOSD is a
systemic inflammatory disease that can be challenging to
diagnose and treat. Its characteristic spiking fevers, arthritis,
rash, and high ferritinemia can elude clinicians. This
report highlights the importance of recognizing AOSD to
initiate early therapy, and the room for additional research
to optimize treatment options.
Acknowledgements: The authors would like to acknowledge
Dr. Melissa Sergi, Dr. Gregory Gaisano, and Dr. Vlad
Dragan for their roles as part of the medical care team. We
would like to thank our patient for providing consent for
this case report.
Ming K. Li, BHSc
Temerty Faculty of Medicine,
University of Toronto
Toronto, Ontario
Calandra Li, MSc
Temerty Faculty of Medicine,
University of Toronto
Toronto, Ontario
Anas Makhzoum, MD
Rheumatology Division,
Trillium Health Partners,
Mississauga, Ontario
Rohan Philip, MD
General Internal Medicine,
Toronto General Hospital
University of Toronto
Toronto, Ontario
Glossary:
a. ESR: erythrocyte sedimentation rate
b. CRP: C-reactive protein
c. ANA: anti-nuclear antibodies
d. RF: rheumatoid factor
e. CT: computed tomography
f. ENA: extractable nuclear antigen
g. ANCA: antineutrophil cytoplasmic antibodies
h. anti-CCP: Anti–cyclic citrullinated peptide
i. CBC: complete blood count
j. NSAIDs: Non-steroidal anti-inflammatory drugs
k. DMARDs: Disease-modifying antirheumatic drugs
References:
1. Yamaguchi M, Ohta A, Tsunematsu T, et al. Preliminary criteria for classification of adult Still's
disease. J Rheumatol. 1992 Mar 1; 19(3):424-30.
2. Magadur-Joly G, Billaud E, Barrier JH, Epidemiology of adult Still's disease: estimate of the incidence
by a retrospective study in west France. Ann Rheum Dis. 1995 Jul; 54(7):587-90.
3. Gerfaud-Valentin M, Jamilloux Y, Iwaz J, et al. Adult-onset Still's disease. Autoimmunity reviews.
2014 Jul 1; 13(7):708-22.
4. Giacomelli R, Ruscitti P, Shoenfeld Y. A comprehensive review on adult onset Still's disease.
J Autoimmun. 2018 Sep; 93:24-36.
5. Kadavath S, Efthimiou P. Adult-onset Still's disease—pathogenesis, clinical manifestations, and
new treatment options. Ann Med. 2015 Feb; 47(1):6-14.
6. Pouchot J, Sampalis JS, Beaudet F, et al. Adult Still's disease: manifestations, disease course, and
outcome in 62 patients. Medicine (Baltimore). 1991 Mar; 70(2):118-36.
7. Franchini S, Dagna L, Salvo F, et al. Efficacy of traditional and biologic agents in different clinical
phenotypes of adult-onset still's disease. Arthritis Rheum. 2010 Aug; 62(8):2530-5.
|
