Spring 2021 (Volume 31, Number 1)
RheumVision:
Harnessing Telemedicine to Improve Access to Care in Rural British Columbia
By Brent Ohata, MD, CM, FRCPC
Download PDF
The current COVID-19 pandemic has resulted in a
widespread embrace of telemedicine inconceivable
prior to the pandemic. Even after the resolution of
the COVID-19 pandemic, ongoing acceptance and usage
of telemedicine will likely persist.
In British Columbia, we are trying to harness this
newfound embrace of telemedicine to establish a video-based
rheumatology hotline for rural physicians, called
RheumVision. Rural physicians simply click on an app link
to set up a video chat room with themselves, the patient and
the rheumatologist on call. Visual data from the encounter
is an improvement on the previous telephone-based hotline
that currently exists in the province. Additionally, the
RheumVision rheumatologist has the option to provide
longitudinal care for the patient until the closest local
rheumatologist can assume care.
This initiative is part of a suite of exciting apps now
available to BC rural physicians. Similar video hotlines also
provide critical care, pediatric, ER, dermatology, maternity,
hematology, thrombosis and pain management advice
on demand, in real-time. More subspecialty pathways will
be added in the future. Beyond the subspecialized education
that occurs, video technology has also facilitated
procedural support. Intensivists have virtually assisted
with the conscious sedation and cardioversion of unstable
patients. RheumVision rheumatologists have coached physicians
through first-time joint aspirations and injections.
As in many parts of Canada, rural British Columbians
frequently face barriers accessing medical subspecialists,
including rheumatologists. Most BC rheumatologists practice
in only a handful of urban locations, and only sporadically
visit smaller, more remote communities via travelling
clinics. Perilous roads, unforgiving employers, limited
finances, and personal struggles all contribute to missed
in-person appointments for rural patients. Improving outcomes
for these patients requires a change in our mode of healthcare delivery. Although increasing rheumatologic
manpower in underserved areas has long been the envisioned
solution to this problem, few gains have ever materialized.
Innovative models of care such as RheumVision have the
potential to lower the barriers to care that many rural patients
face. Instead of travelling hours to see their specialist,
patients can access their rheumatologist at their local health
clinic. Patients are also seen when their schedule permits,
not when the rheumatologist has availability.
History teaches us that, after the Plague of 1347, came
the Renaissance. Without the changes that accompanied
the COVID-19 epidemic, a program such as RheumVision
could never have been implemented. Patients and healthcare
providers alike were more resistant to telehealth one
year ago. All of humanity has suffered as a consequence of
COVID-19. But COVID-19 has also accelerated many necessary
changes in society. One hopes that RheumVision
is the beginning of many good things to come.

Connecting with a family physician and patient on a remote
reserve 14 hours from Vancouver. The patient had a definite
flare of her rheumatoid arthritis, and we were able to advance
care without her leaving her community.
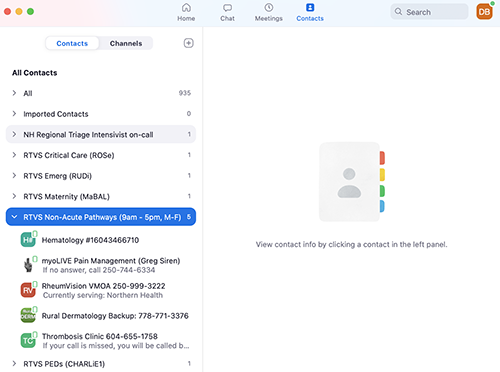
A look at the app now available to all rural BC family physicians.
Brent Ohata, MD, CM, FRCPC
Clinical Assistant Professor,
UBC Division of Rheumatology
Burnaby, British Columbia
|
