Spring 2021 (Volume 31, Number 1)
Addressing Inequity in Northern
Ontario: A Look to the Future
By Sahil Koppikar, MD, FRCPC
Download PDF
Inequity and systemic discrimination have become
front page news and part of dinner-time conversations
in 2020. In healthcare, we have been discussing the
very same topics. Although rheumatology has made great
strides in the last few decades improving the health outcomes
for our patients, inequity amongst certain groups remains.
If we want to address inequity in rheumatology, we
need to examine in depth those who are achieving suboptimal
outcomes, identify the barriers in that population,
and target solutions directly at those barriers.
In Ontario, such an examination turns our eyes
northward.
Northern Ontario is a region of the province where
health equity is often lacking and needs to be addressed
with urgency. Using a rheumatology lens, patients in the
north have reduced access to rheumatology care,1,2 are
more likely to have poorer outcomes,3 experience adverse
events4,5 and are at greater risk of death6 compared to provincial
averages.
There are many causes for these discrepancies, rooted
in the broader social determinants of health, that have a
large impact on health outcomes. Over the past five years,
there has been a big push from government and provincial
organizations to systematically study and plan initiatives to
mitigate some of these barriers in the short and long term.7
While these top-down approaches will impact the system
as a whole, as rheumatologists we can narrow the health
gap with some bottom-up solutions, focused on health
care delivery.
In the CRAJ Winter 2020 issue, Dr. Laurence Rubin
eloquently described one such solution. The Timmins
Arthritis Clinic, in its current format, has been running
since the late 1980s. The success of this clinic was built on
decades of commitment from Dr. Rubin, Dr. Carette, and
the Arthritis Society Advanced Clinical Practitioners in
Arthritis Care, known as ACPACs (Mary Ellen Marcon and
Lynn Richards). Importantly, they created a sustainable
model of care (MOC) that was not dependent on only
one physician. Over the last year, we have added weekly
“direct-to-home” virtual visits that have helped to shorten
the waitlist, allow for urgent consults, and increase the number
of patients who can be assessed. Despite the success
of this model in Timmins, similar siloed programs will be
increasingly difficult to create and maintain. Instead, we
need a holistic and collaborative approach to address gaps
and leverage our voice towards creating lasting systemic
improvement.
To this end, in the summer of 2020, the Ontario Rheumatology
Association (ORA) created a Northern Ontario
Committee that comprises rheumatologists, ACPACs and leaders from the Arthritis Society who are involved in
northern care. This has been instrumental in bringing
people with similar goals and vision together to generate
innovative ideas.
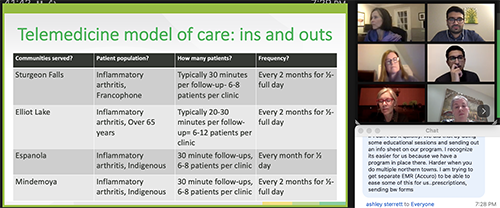
In January 2021, the committee hosted two workshops
to educate ORA members on the “current state of the north”
and to recruit members who are interested in providing
virtual care to northern patients in an ACPAC-physician
model. This MOC already exists, with the ACPACs based in
Sudbury and Thunder Bay. However, with increasing patient
needs and upcoming retirements, it is important that
we sustain the care that is already provided. We are hoping
to leverage new virtual care skills that have been developed
over the pandemic and find members who will be willing to
offer care to patients in northern Ontario.
In recognition of the higher prevalence of Indigenous
populations in northern Ontario, we will be asking all new
“recruits” to complete Indigenous Cultural Safety Training.
8 Indigenous populations have faced various discriminatory
policies that have created inequalities that continue
to affect their health. It is the least we can do to recognize
this, enhance self-awareness, and strengthen the skills of
those who work with Indigenous people.
Over the last few years, we have also seen increased interest
in new graduates setting up practice or travelling
to the North. Two early career rheumatologists, Drs. Saara
Rawn and Matthew Piche, have established permanent
practices in Sault Ste. Marie. Dr. Maysam Khalfan has set
up regional clinics in Kapuskasing and Hearst and plans
on travelling up four times a year to provide care in these
regions. Drs. Elishka Pek and Lauren King are looking to
set up a similar visiting model in Thunder Bay. In Timmins,
we have recruited Dr. Medha Soowamber, who is fluent in
French – a critical requirement in an area where 20% of
people are francophone. This interest, and action, by early
career rheumatologists is encouraging and I hope it is something
that sustains and expands over the coming years.
The long-term vision is to establish a multidisciplinary
model that relies on training local ACPAC/extended-role
practitioners (ERPs) at each major northern hub who can
work alongside rheumatologists that are local, visiting, or
using telemedicine. This model could potentially allow for
central triaging in the north to optimize wait times and
provide an expert local resource to the communities. This
will require creative solutions and new MOCs that do not
currently exist. Earlier in 2020,
Drs. Stephanie Tom (previous
chair) and Rachel Shupak met with the Ministry of
Health to discuss these issues. The Ministry was engaged
and receptive and asked for a proposed business case that
outlines what we envision as the ideal MOC. The ORA
Northern Ontario Committee has been working on the business
plan and is aiming to present it to the Ministry in
the spring/summer of 2021. While we are being pragmatic,
we will aim for the stars and see where that gets us!
At the end of the day, a strategy to address health equity
will require engagement and commitment of stakeholders
and leaders in the North. As Dr. Jennifer Walker (Canada
Research Chair in Indigenous Health at Laurentian University)
put it, “Solutions cannot simply be imported from
the southern part of the province. The landscape – social
and cultural as well as geographic – is totally different.”
But we can all contribute in different ways to narrow the
health equity gap and ensure patients get the care they
need, no matter where they live, who they are, or what they
have.
The ORA Northern Ontario committee workshop on northern virtual care. There was a great amount of interest from both new
and experienced rheumatologists.

Dr. Medha Soowamber (left) and Lynn Richards (right) during
our December 2020 trip to Timmins, in classic 2020 style with
masks!
Sahil Koppikar, MD, FRCPC
Rheumatologist,
Women’s College Hospital, Toronto
Director, Timmins Arthritis Program
Chair, Northern Ontario Committee (ORA)
References:
1. Widdifield J, Paterson JM, Bernatsky S, et al. Access to rheumatologists among patients with newly
diagnosed rheumatoid arthritis in a Canadian universal public healthcare system. BMJ Open. 2014;
4(1):e003888.
2. Badley E, Veinot P, Ansari H, et al. 2007 Survey of Rheumatologists in Ontario. University Health
Network; 2008.
3. Nagaraj S, Barnabe C, Schieir O, et al. Early rheumatoid arthritis presentation, treatment, and outcomes
in Aboriginal patients in Canada: A Canadian early arthritis cohort study analysis. Arthritis
Care Res (Hoboken). 2018; 70(8):1245-50.
4. Widdifield J, Bernatsky S, Paterson JM, et al. Serious infections in a population-based cohort of
86,039 seniors with rheumatoid arthritis. Arthritis Care Res (Hoboken). 2013; 65(3):353-61.
5. Ravi B, Croxford R, Hollands S, et al. Increased risk of complications following total joint arthroplasty
in patients with rheumatoid arthritis. Arthritis Rheumatol. 2014; 66(2):254-63.
6. Widdifield J, Bernatsky S, Paterson JM, et al. Trends in excess mortality among patients with rheumatoid
arthritis in Ontario, Canada. Arthritis Care Res (Hoboken). 2015; 67(8):1047-53.
7. Health Quality Ontario. Northern Ontario Health Equity Strategy 2020. Available at: https://www.hqontario.ca/What-is-Health-Quality/Health-Equity-and-Quality/Our-Work/Northern-Ontario-Health-Equity-Strategy. Accessed February 2021.
8. Provincial Health Services Authority Indigineous Health Program. San’yas Indigenous Cultural Safety
Training 2020. Available at: https://www.sanyas.ca/about-us. Accessed February 2021.
|




