Spring 2021 (Volume 31, Number 1)
Survey Results:
Telehealth Use in Canada
On behalf of the CRA Telehealth Committee
Download PDF
The COVID-19 pandemic has necessitated many
changes in healthcare; for patients with rheumatic
disease this has primarily translated into how patients
are seen by their healthcare providers. While telehealth
and e-medicine existed before, the pandemic has
led to a dramatic shift in how these formats are used. For
this issue’s Joint Count survey, in December 2020, we
reached out to the CRA membership to ask about their
perspectives on telehealth use in Canada. For the purposes
of the survey, “telehealth” encompassed telephone
and videoconference visits.
The first survey question asked whether video and telephone
visits are paid at the same fee as in-person visits
in their province. For both video and telephone visits, approximately
70% responded that they are paid the same
fee as in-person visits. Further to this, 73% agreed that in
the future (post-COVID) telehealth visits should be paid
the same fee as in-person appointments.
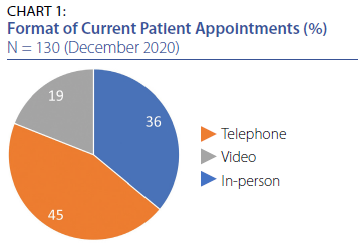
When asked to estimate what percentage of current
patient appointments are conducted via telehealth (e.g.,
telephone or videoconference) vs. in-person visits, taking
the collective average, 36% are in-person visits, 45% via
telephone and 19% via video (refer to Chart 1).
The next question asked “What percentage of new patients
are you seeing via telehealth?” Approximately a
third (30%) responded that they are seeing the majority
of their new patients (>75%) via telehealth. Another 28%
indicated that they saw less than a quarter of their new
patients via telehealth, with 20% saying they saw no new
patients via telehealth.
In terms of being comfortable seeing new patients by telehealth,
only 8% said they were very comfortable. Sixteen
percent (16%) indicated they were comfortable; 27% said
they were somewhat uncomfortable; 13%, neutral; and finally,
35% said they were not at all comfortable.
When asked “which parts of the physical exam do you
incorporate into your telehealth visit, when clinically indicated
(choose all that apply)?” the most common responses
included visual exam for swollen joints (66%); self-exam
for tender joints (60%); dermatologic exam – either real
time or with photos afterwards (57%); and virtual GALS/
pGALS/or other range of motion exam (48%).
As one might expect, there are both benefits and disadvantages
to telemedicine. Indeed, one respondent pointed
out that “When there is no pre-existing relationship, it is
likely harder for patients to have a sense of trust when the
visit is only by phone. From the physician side, there are
many features that you can miss without visual contact of
some sort.” Similarly, another physician commented that
“…it is also difficult to assess patients whose first language
is not English as I am never sure that my questions are understood
even when there is a relative involved acting as a
translator.” Another stated that “Questions and history are
easy by telehealth, but not physical exam which is essential
to complete the initial rheumatology consultation.”
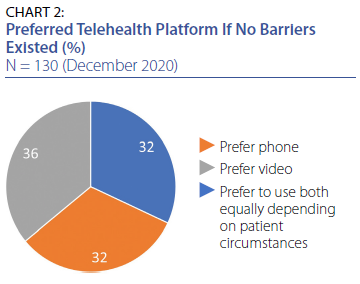
On the other hand, there is also a distinction to be
made between a video visit and a telephone call. One physician
wrote “I see all new patients by video if possible (over
90%). I find telephone consultations much less reliable.”
Others suggested that the technical difficulties of setting
up video calls with patients who are not familiar with the
technology are a significant barrier. Indeed, patient comfort
with technology is a limitation, particularly with video
calls, and there can also be technical barriers such as an
inadequate internet connection. Finally, the lack of a proper
setup and even privacy or noise can be concerns, with
the presence of other members in a household, both for
patients and physicians alike.
Additional barriers mentioned by survey takers included
the lack of administrative support. For example,
adding new ways that patients can be booked adds more
variables to an already taxed system.
Nevertheless, telemedicine can certainly be convenient,
particularly for rural patients in the winter months,
and many reported that their follow-up patients are very happy with virtual visits. The wide variety of responses and
comments in this survey confirm that telemedicine has an
important role in the future of healthcare, though whether
it will be used or not for a specific patient ultimately depends
on the patient, their condition and their unique circumstances.
The CRA Telehealth Committee is working on best
practice recommendations and looks forward to seeing
results from multiple quality improvement and research
efforts assessing telehealth models of care being carried
out by CRA members.
If you have any additional feedback for the CRA, please
contact Sue Ranta at sranta@rheum.ca.
*The response rate to the survey was 130 out of a possible 599, equating to 22%. Approximately 44% of respondents were academic rheumatologists and 43% were community rheumatologists, and among these 24% were both; 14% were pediatric rheumatologists.
|




