Summer 2020 (Volume 30, Number 2)
Glucocorticoid Tapering in Vasculitis
By Arielle Mendel, MD, FRCPC, MSc, on behalf of CanVasc
Download PDF
Treatment of the systemic vasculitides usually requires
initial high-dose glucocorticoids (GC), which must
be tapered over time to avoid toxicity. Recommendations
suggest tapering to 15-20 mg prednisone per day
within 2-3 months of therapy in giant cell arteritis (GCA)1, 2
and ANCA-associated vasculitis (AAV).3 The recently published
PEXIVAS trial demonstrated that, in severe granulomatosis
with polyangiitis (GPA) and microscopic polyangiitis
(MPA), a faster, “reduced-dose” GC tapering protocol
(target 7.5-12.5 mg prednisone daily by 3 months), was
non-inferior to a ”standard” taper (target 15-25 mg daily by
3 months) in terms of global and renal survival, with a lower
risk of serious infections.4
The purpose of this Joint Count survey was to determine
how Canadian rheumatologists taper prednisone in GCA
and AAV, and how many have adopted a “reduced dose”4
tapering strategy in AAV.
Seventy-one Canadian rheumatologists and trainees
completed the survey (13% response rate). The majority
worked in an academic setting (47%), while 32% worked
in the community and 20% in both. Most (73%) have practiced
for ≥5 years, and half (49%) saw patients with vasculitis
at least once weekly.
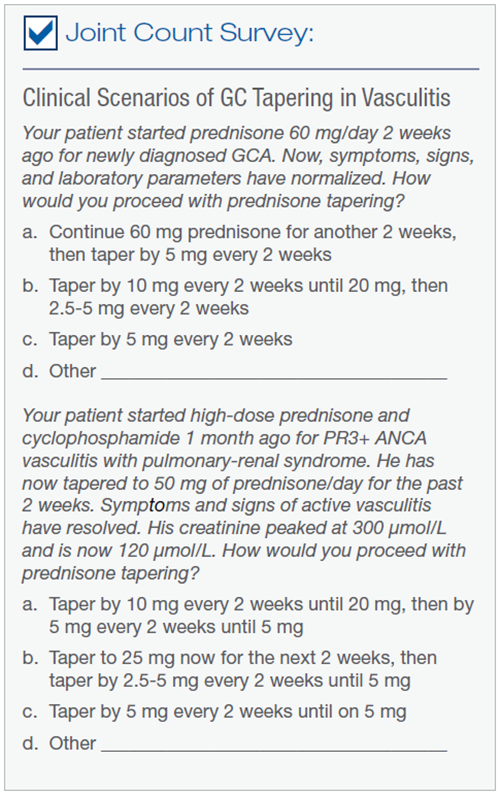
The survey presented clinical scenarios of GC tapering
in GCA and GPA (refer to the panel below). For the
GCA scenario, most (76%) tapered prednisone to reach
the recommended dose of 15-20 mg daily by 3 months1,2
and the remainder tapered more slowly. For the GPA scenario,
most (85%) tapered prednisone in a similar manner
to CanVasc recommendations3 (67%) or following a “reduced-
dose” (PEXIVAS)4 regimen (18%), while 15% tapered
more slowly.
The fact that only a minority of physicians have started
to taper GC in GPA/MPA according to the “reduced-dose”
PEXIVAS regimen4 may be due to the recency of the trials’
publication and/or concern that the study results may not
be generalizable to all severe AAV subgroups. Indeed, respondents
ranked “managing the risk of disease flare” as
the most challenging aspect of GC tapering in vasculitis.
The proportion choosing the “reduced-dose” PEXIVAS vs.
other tapering regimens in the GPA scenario did not differ
significantly according to practice setting (academic vs. all
others), clinical experience (≥ 5 or <5 years in practice), or
frequency of seeing patients with vasculitis (at least once
weekly vs. less often).
The risk of GC-related harm increases with cumulative
GC dose and duration,5,6 and following a GC tapering
schedule is one strategy for minimizing toxicity. The soon-to-be published updated CanVasc recommendations for
management of AAV advocate for timely protocolized GC
tapering, acknowledging the potential need for modifications
according to patients’ clinical status.
The results of this survey are reassuring in that most
clinicians taper GC in vasculitis according to recommendations.
CanVasc would like to thank everyone who participated
in this edition of the Joint Count Survey!
Arielle Mendel, MD, FRCPC, MSc
Vasculitis Fellow, Mount Sinai Hospital
Toronto, Ontario
References:
1. Dasgupta B, Borg FA, Hassan N, et al. BSR and BHPR guidelines for the management of giant cell arteritis.
Rheumatology (Oxford) 2010; 49(8):1594-7. doi: 10.1093/rheumatology/keq039a [published Online First:
2010/04/08]
2. Hellmich B, Agueda A, Monti S, et al. 2018 Update of the EULAR recommendations for the management of
large vessel vasculitis. Ann Rheum Dis 2019 doi: 10.1136/annrheumdis-2019-215672 [published Online
First: 2019/07/05]
3. McGeoch L, Twilt M, Famorca L, et al. CanVasc Recommendations for the Management of Antineutrophil Cytoplasm Antibody-associated Vasculitides. J Rheumatol 2016; 43(1):97-120. doi: 10.3899/
jrheum.150376
4. Walsh M, Merkel PA, Peh CA, et al. Plasma Exchange and Glucocorticoids in Severe ANCA-Associated
Vasculitis. N Engl J Med 2020; 382(7):622-31. doi: 10.1056/NEJMoa1803537 [published Online First:
2020/02/14]
5. Gale S, Wilson JC, Chia J, et al. Risk Associated with Cumulative Oral Glucocorticoid Use in Patients with
Giant Cell Arteritis in Real-World Databases from the USA and UK. Rheumatol Ther 2018 doi: 10.1007/
s40744-018-0112-8.
6. Robson J, Doll H, Suppiah R, et al. Glucocorticoid treatment and damage in the anti-neutrophil cytoplasm
antibody-associated vasculitides: long-term data from the European Vasculitis Study Group trials. Rheumatology (Oxford) 2015; 54(3):471-81. doi: 10.1093/rheumatology/keu366
|
