Spring 2019 (Volume 29, Number 1)
Facilitating Physical Activity Prescription
by Medical Professionals with
Open-access Web-based Resources
By Derin Karacabeyli; Kaila Holtz, MD, MSc; and Kam Shojania, MD, FRCPC
Download PDF
Introduction
Physical inactivity is a global public health problem,1 and
regular exercise is one of the most powerful modifiable risk
factors for the prevention and management of chronic disease.2 Regular physical activity has been shown to reduce
the incidence of cardiovascular disease, stroke, hypertension,
type 2 diabetes, certain cancers, and premature
all-cause mortality.3 In patients with inflammatory arthritis
and osteoarthritis, regular physical activity improves
function, reported pain, and quality of life.4,5 Despite the
abundant evidence supporting the role of regular physical
activity in the prevention and management of chronic disease,
inactivity remains the norm. As of 2013, 78% of Canadian
adults and 91% of youth were not meeting the guidelines
of 150 minutes of moderate intensity exercise and two
strength training sessions per week.6
While patients are more likely to exercise if physical activity
is addressed by their healthcare provider,7 exercise
prescription in the clinical setting has its challenges. Busy
clinicians report barriers such as lack of time, knowledge,
training, and resources.8,9 With www.ExRxMed.com, we hope
to empower all physicians to ask every patient at every visit
about physical activity in an individualized, time-efficient
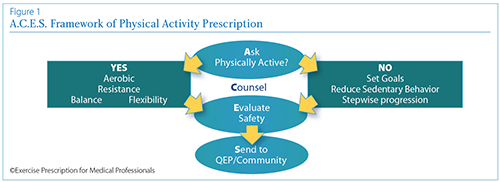
manner. An Overview of the A.C.E.S Framework for discussing
physical activity is shown below (Figure 1).
1) Ask about physical activity.
Start the conversation about physical activity using
non-judgmental language and open-ended questions:
“What do you like to do that is physically active?”
An online physical activity vital sign calculator is integrated
into the website, and we encourage clinicians to
send this to their patients in advance via email. It generates
a printable PDF report that can serve as the basis for your
conversation about physical activity if time permits.
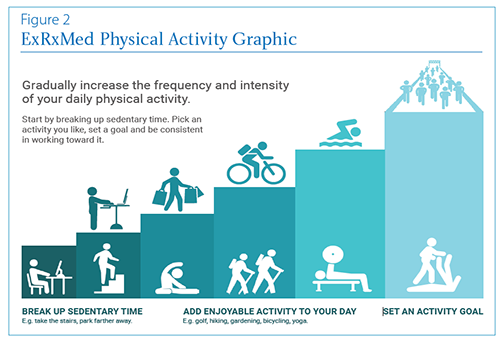
2) Counsel individuals to reduce sedentary time.
If patients are inactive, the first priority is counseling to
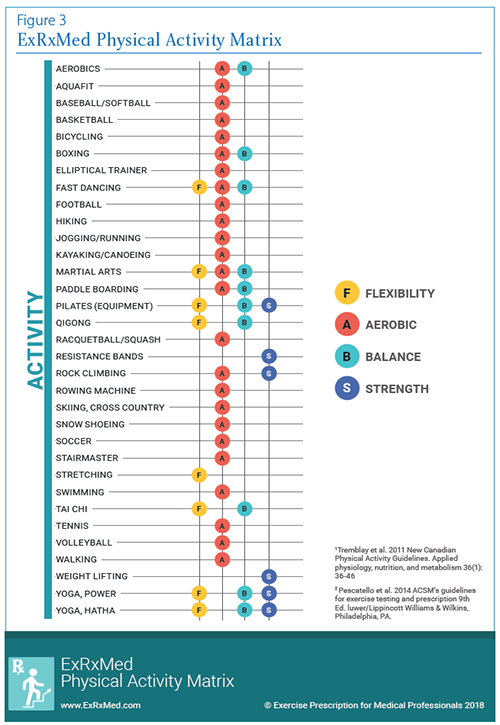
reduce sedentary time (Figure 2). If patients are somewhat
active and motivated, add balance, strength, or flexibility
activities (Figure 3). We have created two resources that illustrate
a simple, step-wise, and safe approach to gradually
increasing the frequency, intensity, and variety of weekly
physical activity.
3) Evaluate for safety.
We have included a link to the “Get Active Questionnaire”10
to enable physicians to screen for patients who may need
further cardiorespiratory investigations prior to engaging
in moderate-to-vigorous exercise.
4) Send to a qualified exercise
professional (QEP), if necessary.
There is a referral form available to encourage
patients to find a qualified exercise professional
to assist them in achieving their goals.
We have listed several Canadian resources and
hope to expand this resource in the future.
Finally, there is a link to the Exercise is
Medicine Physical Activity Prescription Pad
for clinicians who wish to complete a formal
prescription for their patients. Our resources
are meant to be used in combination. We
encourage physicians to incorporate them
into clinical practice in a manner that suits
their workflow, patient population, and
available resources.
Conclusion
Physical activity serves as an invaluable pillar
in the prevention and management of many
chronic diseases, as well as in the enhancement
of quality of life. We have adapted the
five A’s model of behaviour counseling11 to
develop a web-based tool aimed at minimizing
commonly reported barriers to physical
activity prescription. Next steps will involve
validation of our tool through formal research
to evaluate the impact and outcomes
of web-based counseling tools on physician
and patient behaviours. Please contact us if
you are interested in collaborating by visiting
www.ExRxMed.com.
References:
1. World Health Organization. Global Strategy on Diet, Physical Activity and Health: Physical Activity.
Available at http://www.who.int/dietphysicalactivity/pa/en/. Accessed November 3, 2018.
2. Naci H, Loannidis JP. Comparative effectiveness of exercise and drug interventions on mortality
outcomes: Metaepidemiological study. BMJ 2013; 347:f5577.
3. Warburton DE, Charlesworth S, Ivey A, et al. A systematic review of the evidence for Canada’s
Physical Activity Guidelines for Adults. Int J Behav Nutr Phys Act 2010; 7:39.
4. Fransen M, McConnell S, Harmer AR, et al. Exercise for osteoarthrtitis of the knee: a Cochrane
systematic review B J Sports Med 2015; 49:1554-57.
5. Metsios GS, Stavropoulos-Kalinoglou A, Kitas GD. The role of exercise in the management of
rheumatoid arthritis. Expert Rev Clin Immunol 2015; 11:1121-30.
6. Public Health Agency of Canada. How Healthy Are Canadians? A trend analysis of the health of
Canadians from a healthy living and chronic disease perspective. Available at https://www.cana
da.ca/content/dam/phac-aspc/documents/services/publications/healthy-living/how-healthy-canadians/
pub1-eng.pdf. Published April 11, 2017. Accessed November 3, 2018.
7. Grandes G, Sanchez A, Sanchez-Pinilla RO, et al. Effectiveness of physical activity advice and
prescription by physicians in routine primary care: a cluster randomized trial. Arch Intern Med
2009; 169:694-701.
8. Hoffmann TC, Maher CG, Briffa T, et al. Prescribing exercise interventions for patients with chronic
conditions. CMAJ 2016; 188:510-18.
9. Hébert ET, Caughy MO, Shuval K. Primary care providers’ perceptions of physical activity counselling
in a clinical setting: a systematic review. Br J Sports Med 2012; 46:625-31.
10. Canadian Society for Exercise Physiology. Get Active Questionnaire. Available at http://www.csep.
ca/en/publications/get-active-questionnaire. Accessed November 5, 2018.
11. Whitlock EP, Orleans CT, Pender N, et al. Evaluating primary care behavioral counseling interventions:
an evidence-based approach. Am J Prev Med 2002; 22:26-84.
Derin Karacabeyli
Faculty of Medicine
University of British Columbia
Vancouver, British Columbia
Kaila Holtz, MD, MSc
Faculty of Medicine
Division of Physical Medicine and Rehabilitation
University of British Columbia
Vancouver, British Columbia
Kam Shojania, MD, FRCPC
Clinical Professor and Head,
UBC Divison of Rheumatology
Medical Director,
Mary Pack Arthritis Program
Vancouver, British Columbia
|




