Fall 2019 (Volume 29, Number 3)
Launching CBD in Pediatric Rheumatology:
Keeping Your Head Above the Water
By Shirley Tse, MD, FRCPC
Download PDF
It is a transformative time for all rheumatology programs with the launch of Competency by Design (CBD) this summer in July. For some, the change may bring some unnecessary heat and stress above and beyond the sunny skies of summer. CBD aims to move away from a time-based approach, as residents are expected to acquire key competencies in knowledge, skills and abilities as they progress along the developmental stages of their rheumatology training program. At each stage, there will be specific tasks or entrustable professional activities (EPAs) that residents must be able to demonstrate independently. Each EPA is broken down into multiple smaller tasks or milestones that residents can work on and develop to make life more manageable, get coaching feedback, but also progress according to their proficiency. Consequently, this will require teachers and assessors to understand the concepts of CBD and to increase direct observation of specific clinical activities and skills of residents, and to personalize their support and expectations according to each resident’s stage of training, development, progress and proficiency.
There are only three pediatric rheumatology training programs across Canada. With fewer faculty and resources compared to some of our adult rheumatology programs, CBD implementation can be challenging. Change can be difficult but in contrast to the motto of the Borg from Star Trek that “Resistance is futile,” I will share 10 survival tips from our training program at SickKids, University of Toronto, that have helped make the transition to CBD easier, more manageable and kept our heads above the water.
- Inform but do not overwhelm people with CBD. Keep it brief, meaningful and fun! This can be via tip sheets, email blast and videos. For example, we have created an introduction video to understand EPAs. Check it out at www.youtube.com/watch?v=VW69qxd5H6k&feature=youtu.be.
- Set individual tasks to be specific and simple. Some may not want to know the history and theory of CBD and prefer to focus on just what they need to do. Examples include:
- Assessors: 1) Observe; 2) Provide coaching feedback; 3) Document.
- Trainees: 1) Pick EPA ahead of time; 2) Ask for Observation; 3) Ask for feedback.
- Competence committee member: 1) Summarize performance; 2) Assess progress and stage of training; 3) Make recommendations
- Try to keep all assessments uniform. Many different assessment tools excluding EPAs are used by the training program and contribute to the overall evaluation of trainees. By revising the scoring system for all non-EPA tools to the CBD entrustment scale, this allows consistency and avoids confusion for both assessors and learners.
- Yes, there are many EPAs and it is hard to keep track of them sometimes. We have made it more manageable by:
- Having a scheduled “EPA of the week” for trainees to focus on as one of their EPAs to attempt (Photo 1). We have created a map that, if followed, the residents will have completed the minimum targets for all EPAs required by the Royal College standards by the end of their training.
- A reference poster that maps relevant EPAs to specific clinical experiences, which is displayed in clinical areas (Photo 2). Faculty and residents can quickly choose EPAs from the designated list that are relevant to the clinical experience according to the residents’ stage of training (e.g. general rheumatology clinic, subspecialty clinic such as lupus clinic, longitudinal clinic, ward/consults etc.). The process is effective and efficient as we have many different subspecialty clinics, and highlighting relevant EPAs avoids unnecessary stress in scrolling through an exhaustive EPA list.
- Complete EPAs and provide coaching feedback in real time. There is truth to the saying “out of sight, out of mind.” Trying to complete an assessment one week after the encounter can be difficult, and the teachable moment may be lost.
- Clinics are busy. Try to observe the resident with the first or last patient of the day to avoid bias in selecting patient encounters, but also to minimize disruptions to clinic flow.
- Use simple and standardized templates for tasks if possible. This helps to ensure tasks are completed accurately, consistently and efficiently. Some templates we have used include:
- Standardized form and script for presentation of resident performance at competence committee (CC)
- Standardized CC report and recommendations to residents for faculty advisors
- Faculty and trainees are both busy. CBD requires many meetings and feedback sessions. Be flexible with scheduling but consider:
- Bundling CC meetings adjacent to residency program committee (RPC) meetings.
- Ensuring CC meetings are multiplatform so people can at tend in person, by teleconference or by videoconference.
- Scheduling regular faculty advisor feedback sessions into the protected academic half-day. As such, residents have a designated time free from clinical duties to meet with their individual faculty advisors.
- Within the climate of coaching feedback, learners need to acclimatize to receiving constructive feedback, with areas of improvements being discussed each time. This is not a high stakes pass/fail moment, but a framework to continue their development to the standards of the discipline, as well as striving towards their personal best.
- Check in with assessors and trainees regularly to monitor their initiated EPA assessments. Send them a scorecard. Most importantly celebrate and acknowledge their efforts. We have monthly rewards for the faculty or trainees who complete the most EPA assessments (Photo 3).
There is no doubt that CBD requires time and effort from both faculty and trainees. However, in line with quality improvement initiatives, we can make the transition to CBD smoother and seamless by collaboratively sharing CBD resources and survival tips. The ultimate goal is worthwhile, and strives to ensure that graduating residents are competent and have the skills and behaviours to meet the evolving patient needs in addition to optimizing patient outcomes.
Photo 1: Kamela Ramlackhan (program administrative assistant) creating and sending out the “EPA of the week.”
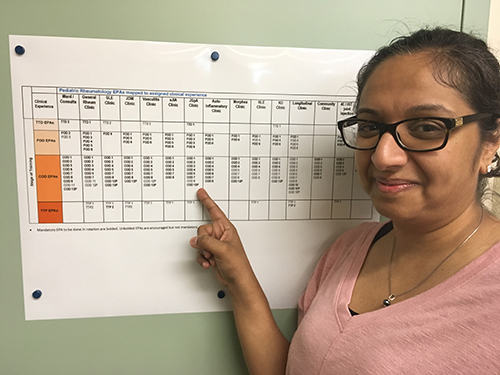
Photo 2: Dr. Piya Lahiry (pediatric rheumatology resident) reviewing and choosing EPAs that can be done during her clinical assignment to juvenile spondyloarthritis clinic.

Photo 3: Dr. Deborah Levy and Dr. Herman Tam celebrate being the first faculty and trainee award recipients for completing the most EPA assessments in July.
Shirley Tse, MD, FRCPC
Associate Professor,
Department of Pediatrics,
University of Toronto
Staff Rheumatologist,
Program Director,
The Hospital for Sick Children (SickKids)
Toronto, Ontario
|




