Fall 2019 (Volume 29, Number 3)
Medical Education 2.0
Making Good Residents Better:
A Follow Up to the CRA ASM Great Debate 2019
By Heather McDonald-Blumer, MD, FRCPC, MSc (HPTE); Mercedes Chan, MBBS, FRCPC, MHPE;
Elizabeth M. Hazel, MD, FRCPC; Marie-Paule Morin, MD, FRCPC, PhD(c); and Raheem B. Kherani, BSc (Pharm), MD, FRCPC, MHPE
Download PDF
Background
Just over 100 years ago, medical education changed dramatically with the publication of the Flexner Report. This resulted in the development of undergraduate and postgraduate medical education as we have known these programs for all of our professional lives.
However, given the need to ensure that all physicians graduating from residency training programs are appropriately competent, over the last 10-15 years, medical educators and patient stakeholders have been re-evaluating how medicine is taught. This has resulted in the worldwide movement towards competency-based medical education (CBME). The goal of training is to ensure physicians are able to do what they need to do, so as to practice all aspects of their specialty effectively and safely.
To align with this outcome-based philosophy, the Royal College of Physicians & Surgeons of Canada has been working with our specialty committee and program directors to develop discipline-specific competency-based medical education curricula. The Royal College has labelled their specific CBME guidelines as Competence by Design (CBD).
As of July 1, 2019, PGY-4s in Canadian rheumatology training programs are now participating in the CBD curriculum, part of the third cohort of programs changing to this new format.
Stages of Training and Entrustable Professional Activities (EPAs)
The practice of rheumatology requires the core knowledge and skills to allow accurate assessment and state-of-the-art treatment of patients with complex rheumatologic diseases. As such, what rheumatology residents must learn will not change, other than the need to incorporate into their learning and practice the scientific and therapeutic advancements that are an intrinsic part of practicing medicine today. The mixture of actually seeing patients, attending rounds and formal teaching sessions, giving presentations and going to our discipline-specific meetings will also not change.
What will change is how residents are assessed. There will be greater emphasis on watching and listening more diligently (direct observation) to ensure that residents can actually do what we think they can do. There will be multiple low-stakes or formative assessments rather than a few major evaluations. Also different from the past will be how this assessment is documented – on electronic platforms and, ideally, in real-time.
Stages of Training
Rheumatology training programs, for the foreseeable future, will remain a two-year postgraduate program following internal medicine or pediatric core training. Those two years will be divided into four stages:
1. Transition to Discipline; 2. Foundations of Discipline; 3. Core of Discipline; and 4. Transition to Practice. These stages focus the resident’s learning from the key issues they need to know in the first several blocks of their rheumatology training through to the important issues that they should address as formal training nears completion and they move toward independent practice.
As clinical supervisors, our expectations of the resident will change as they move across the stages of training. This is not new, but now there are well-articulated benchmarks which will help supervisors determine what specific level of skill a resident should have at a certain stage (timepoint) in training.
EPAs
Perhaps the biggest change or challenge is to understand the new concept of EPAs. The Royal College defines EPAs as the key tasks of our discipline that a resident (or physician) can be expected or trusted to perform in a given healthcare context, once sufficient competence has been demonstrated. The EPAs cover all of the tasks that we do as rheumatologists. To be “entrusted,” the resident must be able to perform the task independently.
There are 24 EPAs for the adult rheumatology residents and 25 for the pediatric rheumatology residents. EPAs are organized according to the resident’s stage of training and increase in complexity over time. Each clinical activity (EPA) is broken down into its key components (known as milestones) which can be used to help supervisors give the resident timely and specific feedback on their performance and identify areas for improvement. Residents will keep track of which EPAs they want a clinical supervisor to review with them each day. In order to determine if a resident is able to complete a specific task independently (autonomously), supervisors will have to directly observe the activity in question.
Examples of EPAs
For a resident as they start their training, an expected task would include: Performing histories and physical examinations in uncomplicated patients with rheumatologic disease, including documenting and presenting findings.
Later in the year, you would expect the resident would be successful in assessing and providing initial diagnosis and treatment plans for patients with uncomplicated rheumatology presentations.
Our program directors have done a huge amount of work over the last several years to prepare their respective schools for CBD. PGY-4 residents are highly engaged in the process. Combined, their efforts are facilitating change. Faculty and clinical supervisors are being asked to integrate the new system into clinical work. While change can be challenging, the bottom line remains the same: All of us who supervise rheumatology residents in our clinical settings will continue to see patients with them, and help residents learn to provide exemplary care to their patients.
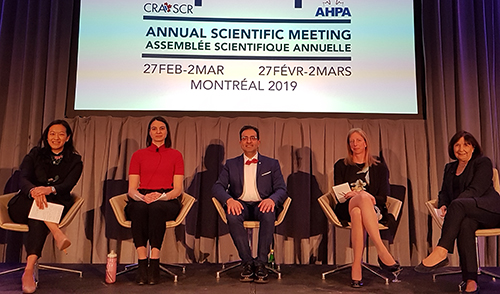
The 2019 CRA ASM Great Debate Team; Pictured from left to right: Dr. Mercedes Chan, Dr. Marie-Paule Morin, Dr. Raheem B. Kherani (Chair), Dr. Elizabeth M. Hazel, and Dr. Healther McDonald-Blumer.
Key Websites and a Few Selected References:
Royal College of Physicians and Surgeons of Canada: Competence by Design. Available at www.royalcollege.ca/rcsite/cbd/competence-by-design-cbd-e. Accessed 28 August, 2019.
Wass V, Van der Vleuten C, Shatzer J, et al. Assessment of clinical competence. Lancet 2001; 357(9260):945-9. Available at www.nuigalway.ie/medical_informatics/documents/Assessment%20of%20clinical%20competence.pdf. Accessed 28 August, 2019.
Flexner A. Medical Education in the United States and Canada. Washington, DC: Science and Health Publications, Inc.; 1910.
The 2019 CRA Great Debate Team:
Heather McDonald-Blumer, MD, FRCPC, MSc (HPTE)
Division Director, Rheumatology
Director,
CBD Planning and Implementation (Medicine),
University of Toronto
Toronto, Ontario
Mercedes Chan, MBBS, FRCPC, MHPE
Program Director,
Pediatric Rheumatology,
University of British Columbia
Vancouver, British Columbia
Elizabeth M. Hazel, MD, FRCPC
Clinical Associate Professor,
Program Director,
Adult Rheumatology,
McGill University
Montreal, Quebec
Marie-Paule Morin, MD, FRCPC, PhD(c)
Division of Rheumatology and Immunology,
CHU Sainte-Justine Department of Pediatrics,
University of Montreal
Montreal, Quebec
The 2019 CRA Great Debate Chair:
Raheem B. Kherani, BSc (Pharm), MD, FRCPC, MHPE
CRA Education Committee Chair,
Clinical Associate Professor,
University of British Columbia
Vancouver British Columbia
|




