Fall 2019 (Volume 29, Number 3)
Running Your First Chart Audit
By Henry Averns, MD, ChB, FRCP (UK), FRCPC
Download PDF
So you want to run a chart audit; maybe because your regulatory college requires it, or maybe because you have a genuine interest in examining aspects of your practice to achieve long-term improvements. Whatever the reason, this is a guide for those of you who are new to the process.
What is a chart audit?
It is a tool for quality improvement to improve processes and outcomes. It is a clinical tool and not a regulatory tool, with the overall aim to review one’s own practice to improve patient safety, effectiveness of treatment, and the patient experience. Areas to examine include:
- The structure of care: e.g. Resources: availability of a therapist, information available for patients.
- The process of care: e.g. Wait times for potential new RA patients to be seen in clinic.
- The outcome of care: e.g. Are patients on NSAIDs assessed for gastroprotection?
Generally the audit compares aspects of one’s medical practice to defined standards. Importantly, this is an iterative process and NOT simply a one-time survey. A properly conducted chart audit will include an intervention, and then a repeat of the cycle. Be warned, this is addictive and once you get the bug you will be doing this annually – we have performed annual audits in our office since 1996!
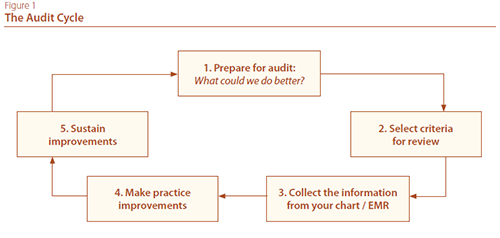
Step by step (refer to Figure 1: The Audit Cycle):
- Identify an area to be audited – are you aware of areas in your practice which may need review? Don’t just choose something you know you do well! Find something where you suspect there is a deficiency.
- Try to find something that will easily incorporate into your current practice – this should not take more than a minute or two per encounter.
- Derive the standards from high quality guidelines e.g. those on the CRA website.
- Define the audit criteria (to compare against the standards). Try to do this in one all-encompassing sentence.
- Collect the data – I find a simple one-sided form with a VERY limited dataset is easiest. You do not want this to eat into your clinical time too much. Another option is to run a query from an electronic medical record (EMR) – that will depend on your confidence in writing queries, and your data discipline. Hence the one side of paper!
- Reflect on the results. Are you achieving the standard? Is there a problem which you need to address?
- Develop action plans to address any deficiencies and institute them. This is the stage most clinicians fail to achieve.
- Repeat the same audit a few months on to find out whether the changes made have improved the process or outcomes.
- Develop a system by which to monitor and maintain the improvements once the audit cycle has been completed. Nowadays with EMRs, structural changes to practice are usually very straightforward.
FAQs
How do I choose something to audit?
Often clinical guidelines are a good source for inspiration. Choosing Wisely Canada defines some hot topics. Another wonderful resource is the “versus arthritis” site which has a large number of audit topics with all of the resources you could need to define the audit standard and get cracking quickly.
Visit the folliwng site for more information: www.versusarthritis.org/about-arthritis/healthcare-professionals/musculoskeletal-impact-toolkit/clinical-audit/.
How do I define the criteria?
Generally you will come up with a statement, for example:
- 100% of patients going on to biologics will have had hepatitis B/C screening.
- 80% of my patients over the age of 60 will be asked about osteoporosis risk factors and the answers clearly recorded in the EMR.
Do I need ethics approval?
A chart audit does not require ethics approval.
How many charts do I need to audit?
Just enough to answer your question! So if ten out of ten times you have failed to record data which you feel should be in the chart, then after only a few charts you will have identified the intervention required.
How good do I need to be at statistics?
You can be as bad as you like. This does not require complex statistics. Generally you are looking at a percentage of charts where you achieve your defined standard.
Henry Averns, MB, ChB, FRCP (UK), FRCPC
Consultant Rheumatologist
Former President,
Ontario Rheumatology Association
Kingston, Ontario
|




