Spring 2016 (Volume 26, Number 1)
A Pan-Canadian Clinical Dataset for Rheumatology
By Vandana Ahluwalia, MD, FRCPC;
Claire Barber, MD, FRCPC, PhD;
Dianne Mosher, MD, FRCPC;
Michel Zummer, MD, FRCPC; and
Sandra Couto, BSc Pharm
Download PDF

Healthcare systems across the globe are undergoing transformations to improve access and quality of care, value for money, and the patient experience. In Canada, the drive towards improving access to care and improving the quality of medical care is building on the foundation of a strong healthcare system. Measurement is an integral part of this process, and defining a common dataset for Canadian rheumatologists will allow us to further drive improvement. Electronic Medical Records (EMRs) and other databases are the necessary tools which have the potential to transform the delivery of care.
Over the last eight years in Canada, the adoption of EMRs by primary-care physicians has more than doubled, moving from 23% in 2006 to 75% in 2014. The adoption of EMRs by community-based specialists has also increased from 28% in 2007 to 70% in 2014.1
The EMR landscape continues to evolve with physicians increasingly realizing the value of implementing an EMR system in their daily practice. Initially, EMR systems were developed for primary-care physicians, and the biggest concern for specialists was the lack of available integrated specialty-specific tools. For hospital- or university-based specialists, there is often no ability to influence or alter templates or data collection within the EMR. Recovery of data is also difficult.
Canadian rheumatologists have taken a leadership role not only in their adoption of EMRs, but in their ability to develop EMR-based tools that allow for more meaningful optimization of these platforms. Clinical forms, disease activity calculators, and capture of patient-reported outcome measurements are some of the important tools that now exist within EMRs thanks to Canadian rheumatologists.
While adoption rates continue to increase, there remains much cross-province variation with respect to how clinical data is captured by clinicians, as well as what data they are collecting. In an effort to qualify and quantify this variability and achieve consensus for harmonization and standardization, the Arthritis Alliance of Canada (AAC) organized two strategic planning meetings bringing together a small working group of rheumatologists with a specialized interest in data collection for clinical care, quality assurance, and research. The first meeting was held in
June 2015 at the University of Calgary; the focused working objectives at hand were to:
• Create consensus that a national framework is needed to stimulate harmonization of datasets amongst provincial groups.
• Identify barriers that may need to be overcome to initiate the discussion around an approach to national
harmonization of data collection.
• Define the minimum rheumatology clinical data sets to be collected cross-provincially.
• Agree on rheumatology indicators (patient care and system indicators) that can easily be captured and reported within EMR and other data platforms.
• Determine resources needed to support this work.
This initial strategy meeting was instrumental in confirming the need for standardization of a rheumatology-specific core dataset.
Taking advantage of the excitement and engagement coming out of the June meeting, the working group immediately planned to reconvene in October 2015, at the AAC Annual Meeting in Kananaskis, Alberta. The second meeting included an expanded group of stakeholders, helping to further define the approach to a pan-Canadian clinical dataset in rheumatology. In preparation for the October meeting, a survey was conducted amongst major investigator-led registry initiatives in Canada to better understand current data-collection
methods. Additionally, data was collected to outline the EMR landscape in Canada, and the ability for data to be accessed and retrieved through EMRs. The October meeting shared key findings from these assessments and identified opportunities to maximize existing tools. Moreover, the meeting established an initial framework towards a pan-Canadian clinical dataset for rheumatology, identifying key elements that should be considered in the formation of the core clinical dataset.
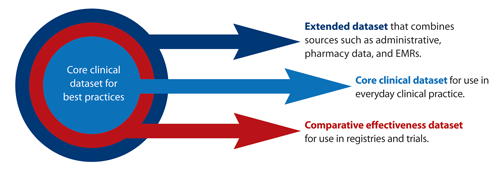
The initial framework put forward for review and
development considers three breadths:
• Core Clinical Dataset for Best Practices
A core clinical dataset recommended for data collection in everyday practice by all Canadian rheumatologists. This includes such data as tender and swollen joint counts, calculated measures of disease activity, and functional status. This dataset will be used in new models of care and will
be based on clinical practice guidelines in rheumatology.
• Comparative Effectiveness Dataset
An expanded clinical dataset that builds on the core clinical dataset for use in registries and clinical trials to support research and improve clinical practice. This includes such data as enhanced adverse event reporting, quality-of-life measures, patient-reported outcome and experience measures, as well as work productivity measures.
• Extended Dataset
A linked dataset that combines data from other sources such as administrative data that reflects health resource utilization (e.g., total physician visits, procedures,
imaging, hospitalizations) and costs.
Final efforts are underway to re-group at the 2016 CRA Annual Scientific Meeting (ASM). The initial working
committee will be expanded to broaden stakeholder participation thereby increasing the awareness and understanding of what data variables are being collected within provinces and the national consensus for standardization of a rheumatology-specific core dataset.
Click here to view larger version of the dataset
Reference
1. National Physician Survey. 2014. National Results by FP/GP or Other Specialist, Sex, Age and All Physicians. Available at: www.nationalphysiciansurvey.ca/wp-content/uploads/2014/11/2014-National-EN.pdf.
Vandana Ahluwalia, MD, FRCPC
Vice-President,
Canadian Rheumatology Association
Corporate Chief of Rheumatology,
William Osler Health System
Brampton, Ontario
Claire Barber, MD, FRCPC, PhD
Assistant Professor,
Division of Rheumatology,
Department of Medicine,
University of Calgary
Calgary, Alberta
Dianne Mosher, MD, FRCPC
Professor of Medicine,
Chief,
Division of Rheumatology,
University of Calgary
Calgary, Alberta
Michel Zummer, MD, FRCPC
Chief of Rheumatology,
CH Maisonneuve-Rosemont
Associate Professor,
Université de Montréal
Montreal, Québec
Sandra Couto, BSc Pharm
Director,
Ontario Best Practices Research Initiative
Partnerships & Stakeholder Relations,
Toronto General Hospital Research Institute
Toronto, Ontario |

