Spring 2015 (Volume 25, Number 1)
Does This Patient Have IgG4-related Disease?
By Luke Chen, MD, FRCPC, MMEd
Download PDF
Case: A 72-year-old woman of East Indian descent presents with nephrotic range proteinuria of 7.2 g/day and an albumin/creatinine (ACR) ratio 1,360 mg/mmol creatinine. A renal biopsy is consistent with membranous glomerulonephritis (MGN). She has a long history of unusual clinical problems starting with a pancreatic mass at age 48. Histology of the Whipple’s resection revealed an atypical lymphocytic infiltrate with no evidence of malignancy; 15 years later, small bowel biopsies for workup of anemia showed a similar atypical T-lymphocyte infiltrate. At age 67, she had autoimmune pancreatitis responsive to steroids as well as bilateral parotid and salivary gland swelling. Excisional salivary gland biopsies revealed “an intense lymphoplasmacytic infiltrate with fairly numerous germinal
centres…a moderate degree of background fibrosis and sclerosis.” The patient was diagnosed with Mikulicz’ disease.
Her recent bloodwork shows eosinophilia 1.9 giga/L, C-reactive protein (CRP) 5.2 mg/L, negative anti-nuclear antibodies (ANA),
low albumin 25 g/L, elevated total protein 91 g/L with increased gamma globulins 27 g/L (normal 7-14 g/L) in a polyclonal pattern with increased immunoglobulin G (IgG) 41 g/L (normal 6.3-18 g/L). She has been referred to address the question of whether there is a systemic disorder unifying the present renal disease with her prior medical history, and whether a unifying diagnosis might inform the optimal systemic therapy for her MGN.
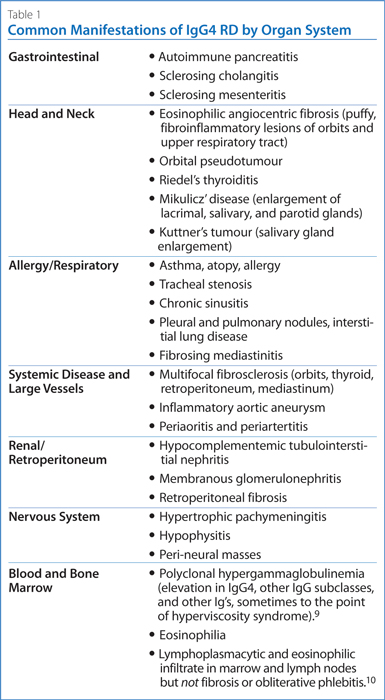
IgG4-related disease (IgG4-RD) is a fibroinflammatory disorder typically associated with tumefactive (puffy) swelling of glandular tissues, with fibrosis and infiltration of affected organs by polyclonal lymphocytes, IgG4+ plasma cells, and eosinophils. About 70% of patients also have elevated serum IgG4 levels. Nearly any organ system can be involved, but like the non-caseating granulomas of sarcoidosis, the histological findings are very similar throughout diverse tissues: storiform (matted and irregularly whorled) fibrosis, obliterative phlebitis, lymphoplasmacytic infiltrate, and eosinophilia. IgG4-RD has been shown to be the underlying cause of numerous diseases which were previously thought unrelated, such as autoimmune pancreatitis,1 Mikulicz’ disease, and multifocal fibrosclerosis. Table 1 lists other manifestations.
This concise review focuses on three questions:
• When should I suspect IgG4-RD?
• How do I approach diagnosis of IgG4-RD?
• How do I treat IgG4-RD?
A number of detailed reviews are recommended for further reading.2-4
When should I suspect IgG4-RD?
Patients typically present with a subacute course, many with chronic unrecognized disease manifestations. The most common disease features are autoimmune pancreatitis, sialoadenitis, lacrimal gland involvement, and retroperitoneal fibrosis. One third of patients have associated atopy, asthma, and eosinophilia.5 This case illustrates classic manifestations and the likelihood of IgG4-RD is extremely high. Her features of eosinophilia, polyclonal hypergammaglobulinemia, increased IgG, modestly elevated CRP, and negative or weakly positive autoantibodies are also consistent with IgG4-RD.
How do I approach the diagnosis of IgG4-RD?
When a case is suspected, the diagnostic tests in Table 2 should be considered. Most important is pathologic review of the tissue specimens. In many cases, archived tissue samples are available; if not, then the most affected organ with lowest risk of morbidity from biopsy should be sampled. 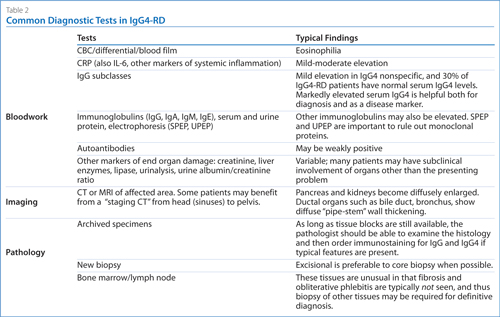
Click here to view larger version of the table
Excisional biopsy is preferred over a core biopsy. Minor salivary gland biopsy can be considered in those patients where a biopsy of other affected organs (such as retroperitoneal fibrosis) requires laparotomy or is otherwise too high-risk. If histologic findings are suggestive of IgG4-RD, immunostaining for IgG and IgG4 should be done (Figure 1).
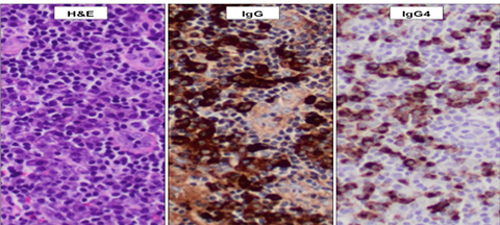
Figure 1. Lymph Node Biopsy, 200 x magnification. Left: a dense infiltrate of lymphocytes and plasma cells (“lymphoplasmacytic”). Middle: many IgG positive plasma cells. Right: many IgG4 positive plasma cells, > 100/high powered field and IgG4/IgG ratio > 40%. (Photo courtesy of
Dr. Graham Slack, BC Cancer Agency).
The International Consensus Criteria6 are applied, wherein for most tissues, an IgG4 count > 50 hpf-100/hpf, and IgG4/IgG ratio > 40% with appropriate histologic findings, is considered diagnostic. Increased IgG4 positive plasma cells are not in themselves specific, and can be found in many “mimickers” of IgG4-RD such as Sjögren’s syndrome, lymphoma, other malignancies, vasculitis, and Castleman’s disease. Classic autoimmune pancreatitis with typical radiologic findings is the one situation where histologic confirmation of diagnosis may not be required.7
The patient’s excisional salivary gland biopsy from 1996 was reviewed and confirmed “a prominent lymphoplasmacytic infiltrate associated with prominent fibrosis. The number of IgG4-positive plasma cells is increased, and there are multiple high power fields that contain more than 100 positive cells. The IgG4:IgG ratio is greater than 40%.” Bloodwork revealed markedly elevated serum IgG4 of
25.7 g/L with other subclasses normal or slightly elevated (normal
< 1.25 g/L). The pathology and lab tests confirm the diagnosis of IgG4-RD.
How do I treat IgG4-related disease?
Treatment is aimed at reducing symptoms, preventing further organ damage, and stabilizing fibrosis (which is typically not reversible). Initial treatment is usually with prednisone 1 mg/kg, with an 80% response rate reported.8 The main toxicity is new or worsening diabetes, since many of these patients have pancreatic impairment to begin with. B-cell depletion with rituximab (1 gram IV Q2 weeks x 2 doses) is very effective, through ablation of the short-lived plasma cells producing IgG4.11 Duration of remission is variable, however, and many patients require re-treatment. The standardized IgG4-RD Responder Index can be used to monitor patients.12 Patients with markedly elevated serum IgG4 at baseline have a convenient and non-invasive means of monitoring, although relapses have been known to occur even with normal serum IgG4. Plasmablast flow cytometry is under investigation as a more sensitive marker of disease activity.13
This patient had an excellent response to prednisone 1 mg/kg
x 4 weeks followed by a slow taper. Because of the extent of her disease burden and risk of progression to end stage renal disease, she was also given
rituximab 1 gram IV x 3 doses. She remains in remission, with normal eosinophils, serum IgG and IgG4, and ACR on maintenance prednisone 5 mg/day.
References & Suggested Readings
For further information, please contact lchen2@bccancer.bc.ca.
1. Kamisawa T, Funata N, Hayashi Y, et al. A new clinicopathological entity of IgG4-
related autoimmune disease. J Gastroenterol 2003; 38(10):982-4.
2. Stone JH, Zen Y, Deshpande V. IgG4-related disease. N Engl J Med 2012; 366(6):539-51.
3. Kamisawa T, Zen Y, Pillai S, et al. IgG4-related disease. Lancet 2015 [epub ahead of print].
4. Mahajan VS, Mattoo H, Deshpande V, et al. IgG4-related disease. Annu Rev Pathol 2014; 9:315-47.
5. Della Torre E, Mattoo H, Mahajan VS, et al. Prevalence of atopy, eosinophilia, and IgE elevation in IgG4-related disease. Allergy 2014; 69(2):269-72.
6. Deshpande V, Zen Y, Chan JK, et al. Consensus statement on the pathology of IgG4-related disease. Mod Pathol 2012; 25(9):1181-92.
7. Shimosegawa T, Chari ST, Frulloni L, et al. International consensus diagnostic criteria for autoimmune pancreatitis: guidelines of the International Association of Pancreatology. Pancreas 2011; 40(3):352-8.
8. Masaki Y. Glucocorticoid Treatment in IgG4-RD. Presented at the International Symposium on IgG4-RD and Associated Conditions. Honolulu, Hawaii, Feb 19, 2014.
9. Chen LY, Wong PC, Noda S, et al. Polyclonal hyperviscosity syndrome in IgG4-related disease and associated conditions. Clinical Case Reports 2015 Feb 2 [epub ahead of print].
10. Cheuk W, Chan JK. Lymphadenopathy of IgG4-related disease: an underdiagnosed and overdiagnosed entity. Semin Diagn Pathol 2012; 29(4):226-34.
11. Carruthers MD, Topazian MD, Khosroshahi A, et al. Rituximab for IgG4-Related Disease: A Prospective Clinical Trial. Arthritis Rheum 2013; 65(Suppl 10):2649.
12. Carruthers MN, Stone JH, Deshpande V, et al. Development of an IgG4-RD Responder Index. Int J Rheumatol 2012; 2012:259408.
13. Wallace ZS, Mattoo H, Carruthers M, et al. Plasmablasts as a biomarker for IgG4-related disease, independent of serum IgG4 concentrations. Ann Rheum Dis 2014; 74(1):190-5.
Luke Chen, MD, FRCPC, MMEd
Clinical Assistant Professor,
Division of Hematology,
University of British Columbia
Hematologist,
Vancouver General Hospital
Vancouver, British Columbia |



